As we count down to 2021 amidst the raging second wave of Covid-19, all Malaysians could sense that we are in a bad situation and many of us have suffered for it, some catastrophically. It is time to take stock of our situation, and to look ahead in 2021, how we individually and how our government representing us collectively, can progress against Covid-19.
The goal in 2021 has to be zero new cases, so that our kids can go back to school, businesses can start thriving and more adults can go back to work.
My motivation for writing this as a retired doctor and statistician is to counter the widespread misinformation and the whiff of anti-vaxxer sentiment, both spreading through social media (I don’t have any such accounts, even then some still got through to me from the various chat groups I join). Clear science- and fact-based communication has to be an important component of any response to this terrible epidemic.
The Past: Covid-19 in Malaysia Since The First MCO In March 2020
Let’s start by looking back at the past nine months to understand how we arrive at our present situation. The charts below show the daily cases and cumulative cases reported since March.
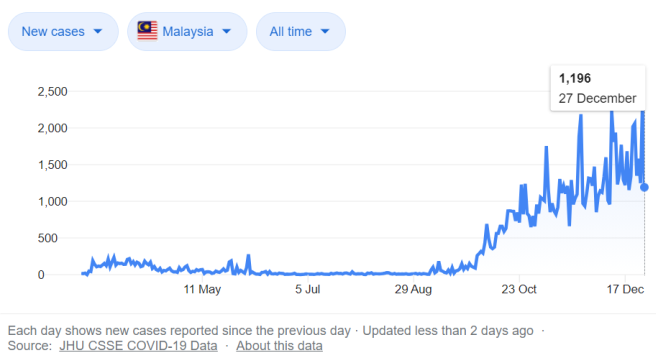
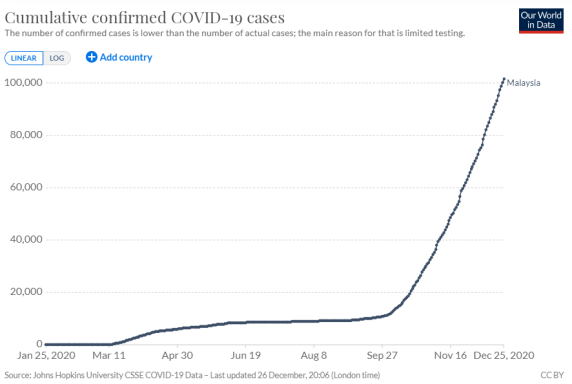
The first spike in cases in March which prompted nation-wide lockdown was followed by several months of single digit counts daily (and MCO was happily lifted) until September when the second wave took off and it is still raging. As a concerned citizen, you must be wondering what happened? Did we get it wrong?
All experts agree that a lockdown is not and cannot be the solution; nobody could tolerate indefinite lockdowns and one among other objectives of a successful containment strategy is indeed to avoid lockdowns.
A lockdown is intended to buy time, time required to understand the characteristics (technically what experts call the transmission dynamics) of the epidemic, and thereby to formulate our strategy and to prepare accordingly.
Even in February to March, when SAR-CoV-2 (the virus which causes the disease Covid-19) was just spreading from Wuhan to the rest of the world, it was predicted based on early data [1,2], that the epidemic will not go away like SARS did in 2003. By May [3], it was all but confirmed that a substantial number of people had asymptomatic Covid-19 and they are infectious during the asymptomatic/ pre-symptomatic phase of the infection.
Both these characteristics were in sharp contrast to SARS. And in common with SARS, Covid-19 was prone to super-spreading, meaning a few infected persons are sufficient to spread the infection to many people in a community (technically, over-dispersion or transmission heterogeneity).
Many countries in the Asia Pacific [4,5] had understood this and adopted aggressive suppressive measures, the so-called “Zero Covid-19” strategy. An extreme example of this was implemented in Qingdao, China, where after initial detection and tracing of 14 cases, the city of 10.9 million people was in lockdown for five days in order to get everybody tested [6].
The strategy paid off for these Asia Pacific countries, they were able to avoid repeated large scale lockdowns, schools and businesses have remained open (and even social life has returned to normal, though borders remained closed) since the initial lockdown beginning of the year.
The alternative is mitigation strategy, just slowing down the infection rate but not sufficient to eliminate community transmission, which many countries outside Asia adopted, perhaps unwittingly for lack of will or understanding. They paid the price of recurrent disruptive lockdowns, economic slowdown and heavy Covid-19 related health burden.
So what did we do in the months after the first lockdown and before the second wave? Did we resolve to pursue a Zero Covid-19 strategy, and throw all we could muster at it? We have certainly ramped up our testing capacity (almost 50,000 tests per day now, thanks to the availability of low-cost antigen tests). However, was our surveillance effective in pinpointing local outbreaks? Was our test and trace system up to it? Did we aggressively deploy targeted lockdowns?
My suspicion is that even if we had intended to pursue a Zero Covid-19 strategy, it probably wouldn’t have worked because of the transmission risk posed by the large number of foreign workers in Malaysia (many of whom are undocumented) living in crowded unhygienic conditions. Indeed, a friend from Singapore had warned in March, when Singapore was battling the outbreak among its foreign workers, that Malaysia will certainly meet the same fate but on a larger scale unless it begins to address this risk.
The Present, And What Lies Ahead in 2021
There is so much water under the bridge. At this stage of the epidemic, the window of opportunity to implement a Zero Covid-19 strategy has long closed — which brings us to the present, in the midst of a raging second wave, which is no longer suppressible.
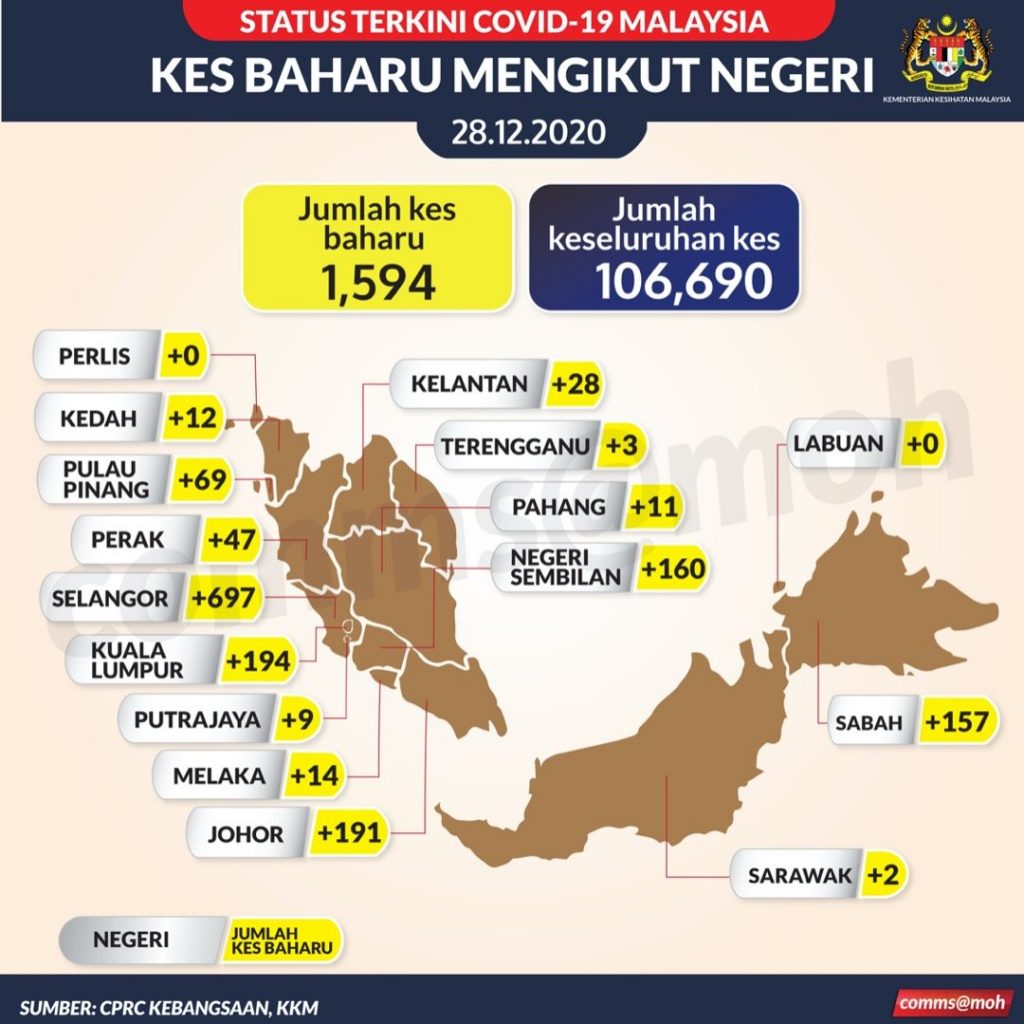
Let’s take stock of our current situation before moving on. Our government reported these statistics yesterday: There were 1,594 new cases on 28 Dec 2020. Cumulatively, 106,690 people in Malaysia have been infected, with 455 deaths. Selangor, KL and Sabah are the worst hit states. But of course we know these numbers are misleading, which raises two questions:
- How many Malaysians really have been infected (incidence)? The actual number infected is much higher (because we don’t test all), typically 10 to 15 times higher [7], so there are likely about 1 to 1.5 million Malaysians infected by now, and counting.
- And how many have died? For the same reason, there are many more deaths attributable to Covid-19 than are reported, the so-called excess deaths [8]. This is as high as 100 excess deaths per 100,000 population (40% higher than usual) in worst affected countries with uncontrolled Covid-19. Assuming the excess death rate is only 25 per 100,000 people in Malaysia, that means every week, about 150 Malaysians would die for a Covid-19 related cause. Now that would be a pretty heavy toll, and would add an urgency to how we are currently handling this epidemic.
Malaysians must face up to reality — Covid-19 is here to stay and there is little chance now it could be suppressed with current response measures.
It has already exacted a heavy toll on us economically (World Bank has forecasted our GDP will shrink by 4.9% this year), and likely a heavy health burden too.
Mitigation is the only option left, and here we have good news. We now have several vaccines, two mRNA vaccines from US, three vector vaccines from Europe, Russia and China, and two Chinese old-fashion inactivated virus vaccines. A vaccine is just a way of getting us all exposed to a component of the virus (the so-called immunogen which induces a protective immune response) without causing the viral illness.
And fortunately, early data from several trials, completed in record time, have found them safe and effective (data pending for some of the vaccines mentioned), at least in the short term, longer term data are still out. Another record is this is the first time mRNA and vector technologies are used as vaccines.
The public however should be assured that it is by no means the first time these technologies are being used on humans. mRNA and vector-based therapies have been in use since 2012 to treat patients with cancers, inherited immunodeficiencies, metabolic, eye, neuro-muscular diseases, even hypercholesterolemia.
Just a few months ago, it wasn’t a certainty at all a vaccine could be available so soon. This goes to show when the will is there among advanced countries, their scientific ingenuity and resources will be brought to bear to solve any technical problem in record time. Sad to say, we couldn’t do the same for infectious diseases exclusive to developing countries, such as dengue which Malaysia has suffered recurrent outbreaks since the Second World War, and Ebola is still raging in parts of Africa.
There will be many challenges ahead with vaccines. Will we obtain sufficient supply to meet our need? Much of the vaccine stock has been bought up by rich countries. Who among us should receive the vaccine first? Shouldn’t the taxpayers pay for the vaccine for everyone? What about foreign workers? They provide the crucial input in our low-cost labour dependent economy.
How can the vaccine intended for all of us be distributed timely, unlike vaccines for newborns and flu shots for elderlies which are required by only a small fraction of the population? Pharmacists and nurses will need to be roped in to administer the vaccine to so many people quickly. I hope our government will be able to get the job done effectively and timely in 2021.
Post-Vaccine Future
Will Covid-19 go away after most of us are vaccinated like SARS did in 2003? Or will it become persistent or endemic in our community, like dengue? Three factors will determine the outcome: immune response to the vaccine, waning immunity over time and immune escape [9].
Covid-19 will become endemic in our community if many people fail to achieve an adequate immune response or the initial protective response to the vaccine declines over time, both are unlikely. Less certain is the third factor, immune escape, whereby the virus mutate and evolve (technically called antigenic drift) such that existing vaccines no longer work. Time will tell.
References:
1. Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N Engl J Med 2020;382:1199-1207
2. Anderson RM, Heesterbeek H, Klinkenberg D, Hollingsworth TD. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet Published Online March 6, 2020
3. Cheng HY, Jian SW, Liu DP, Ng TC, Huang WT, Lin HH; Taiwan COVID-19 Outbreak Investigation Team. Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan and Risk at Different Exposure Periods Before and After Symptom Onset. JAMA Intern Med. 2020;180(9):1156-1163. Published online May 1, 2020. Corrected on September 8, 2020.]
4. Patel P, Sridhar D. We should learn from the Asia–Pacific responses to COVID-19. Lancet Reg Health West Pac. 2020.
5. Summers J. Cheng H.-.Y. Lin H.-.H. et al. Potential lessons from the Taiwan and New Zealand health responses to the COVID-19 pandemic. Lancet Reg Health West Pac. 2020.
6. Xing, Yuhan et al. Rapid Response to an Outbreak in Qingdao, China. N Engl J Med 2020; 383: e129.
7. Pullano, G. et al. Under-detection of cases of COVID-19 in France threatens epidemic control. Nature (2020).
8. Viglione G. How many people has the coronavirus killed? Nature. 2020.
9. Jeffrey Shaman, Marta Galanti. Will SARS-CoV-2 become endemic? Science 30 Oct 2020: Vol. 370, Issue 6516, pp. 527-529.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.





