KUALA LUMPUR, May 18 – The Malaysian AIDS Foundation (MAF) is seeking to bolster their online platform, JomPrep, to help individuals who suffer from severe internal stigmatisation, according to Prof Dr Adeeba Kamarulzaman, chairman of the foundation.
“We really want to strengthen our online JomPrep. There are still some glitches with it. By giving information online, you can order the test and then we will connect you to the nearest provider where there is treatment or prevention,” Dr Adeeba said at the MAF’s Aidilfitri Open House and 30th Anniversary Celebration on Sunday.
“I think this is the way to go for those who suffer from heavy internal stigmatisation. Do it as digitally as possible or virtually as possible.”
JomPrep is designed to help people access pre-exposure prophylaxis (PrEP), which is a medication regimen that can significantly reduce the risk of HIV transmission. The platform provides essential information and assistance to individuals who are seeking to prevent the spread of HIV, including testing, treatment, and prevention options.
Unfortunately, many people from stigmatised and hard-to-reach populations, like men who have sex with men (MSM), face significant stigmatisation and discrimination, which can make it difficult to seek out the help they need. By enhancing JomPrep’s capabilities and making it more accessible, the MAF hopes to provide a more comprehensive solution to this issue, Dr Adeeba said.
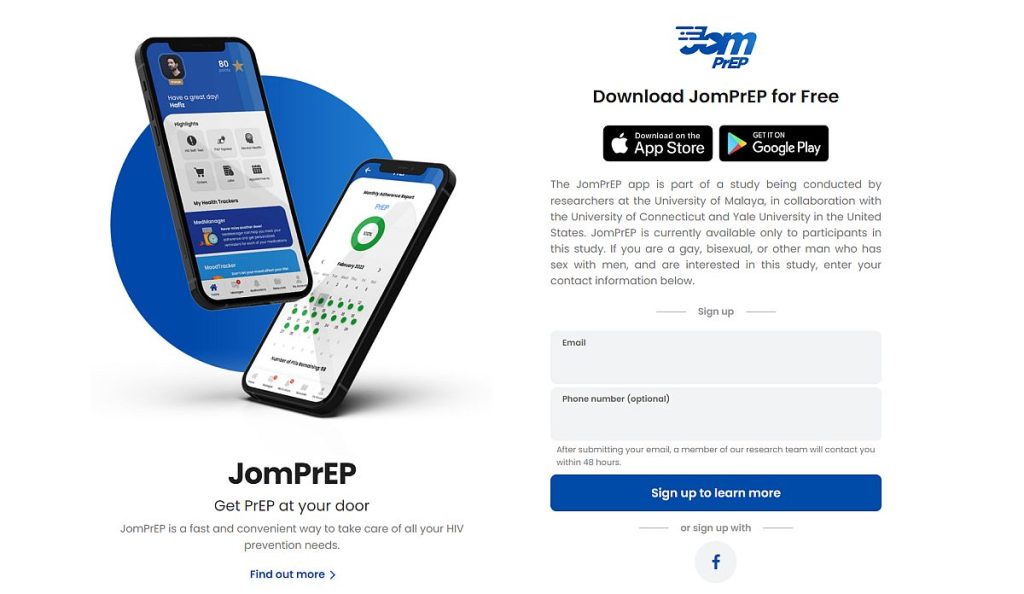
JomPrEP is currently available in the form of a mobile application that can be downloaded from either the Apple store or the Google Play store. However, as stated on its website, the application is still undergoing a research study led by the University of Malaya, in partnership with Yale University and the University of Connecticut. As such, it is only accessible to individuals participating in the study.
The JomPrEP app is an example of mobile health (mHealth), a promising and cost-effective strategy for reaching stigmatised and hard-to-reach populations such as MSM and linking them to care.
In addition to their online JomPrEP platform, MAF community partners conduct outreach programmes to tackle HIV in areas that may not have internet access, particularly in rural areas, Dr Adeeba said.
“That is the importance of having our community partners. They do go out even into rural areas, of course, not as intensively, but that’s the importance of having people on the ground, our community partners beyond KL.
“We’re very lucky to have them, and most of them come from the community. I think that has been the strength of the HIV response all over the world; it is the community response that makes it. As I said in my speech, I think this is something that Malaysia as a country can learn from. The importance of community health workers to undertake projects, especially those that are highly stigmatised, but they require training, funding, and structure. That is where MAF and the Malaysian AIDS Council (MAC) come in; we provide the structure, the oversight on how finances are spent, and it is a less expensive way of doing things, and possibly more effective.
“So, I think that is one thing we are very proud of, working together with the community and, of course, our corporate partners and the Ministry of Health (MOH),” said Dr Adeeba, who is the immediate past president of the International AIDS Society (IAS).
Dr Adeeba highlighted that stigma and discrimination pose significant challenges in achieving the HIV testing, treatment, and viral suppression targets set by the Joint United Nations Programme (UNAIDS).
UNAIDS has updated their global AIDS targets from 90-90-90 to 95-95-95 for their 2025 AIDS targets. This means that 95 per cent of people living with HIV should know their status, 95 per cent of those who know their status should receive treatment, and 95 per cent of those receiving treatment should have suppressed viral loads – the amount of HIV in the blood of someone who has HIV.
“Several countries with higher infection rates than Malaysia have achieved the 95-95-95 targets. It is very possible for Malaysia to achieve all these goals to end AIDS. However, the challenges of stigma and discrimination make it more difficult than it should be.
“For example, an NGO from Negeri Sembilan told me that while they can conduct testing, some people who test positive are still afraid to come forward to receive treatment. Patients may feel shy, scared, or face other barriers. These are the problems we need to address,” said Dr Adeeba, who is also the director of the Centre of Excellence for Research in AIDS (CERiA) at the Faculty of Medicine, University of Malaya.
According to the 2021 Malaysia Stigma Evaluation Survey (MySES), internalised stigma remains a significant challenge for people living with HIV (PLHIV), with 70.1 per cent of respondents reporting feelings of shame due to their status.
The survey also found that almost half of the respondents reported experiencing some form of stigma or discrimination within health care settings. Among the types of discrimination encountered were being advised not to have sex because of their HIV status (46.52 per cent), avoidance of physical contact due to their status (6.23 per cent), and being talked about negatively or gossiped about because of their status.
According to Dr Adeeba, timely HIV diagnosis is crucial for providing prompt treatment to individuals and reducing their viral loads to undetectable levels. This not only prevents the spread of HIV but also enables patients to have unprotected sex.
“What is important now is that we diagnose a person suffering from the HIV disease as quickly as possible so that we can treat them as quickly as possible because with treatment, the virus load in their body will decrease to an undetectable level. If it reaches undetectable levels, they (the patient) will not infect other people.
“Advances in the science of HIV treatment and prevention over the past two or three decades have been significant.
“The patient life expectancy, if treatment is started at an early stage, is the same as those who are not infected. Treatment has also become much simpler. While patients used to take more than 26 pills three times a day, now they can take one pill once a day, which combines three types of medication. In Malaysia, patients may still need to take two pills, but the advantages compared to three decades ago are significant,” Dr Adeeba said.
“The concept of Undetectable Equals Untransmittable (U=U) means that if the HIV level in the body is very low and cannot be detected with a normal test, sexual relations between partners and even between pregnant mothers and their babies will not infect them, and sex without a condom will not infect. That’s why we continue to work hard to diagnose people with HIV as quickly as possible and help them achieve U=U levels.”
For people who do not have HIV but are at a high risk of contracting HIV, Dr Adeeba said they should consider taking pre-exposure prophylaxis (PrEP) medication which can reduce their risk of getting HIV from sex or injection drug use.
“If a person is at high risk of being infected but hasn’t yet contracted the virus, we advise them to start taking PrEP medication,” Dr Adeeba explained. While the exact figures for PrEP uptake in Malaysia are not available, Dr Adeeba noted that the take-up rate is increasing, even though only 0.3 per cent of Malaysians are diagnosed with HIV.








