KUALA LUMPUR, May 13 — Despite several government hospitals reporting Covid-19 clusters among health care workers, Universiti Malaya experts believe adequate support and guidelines are in place to prevent infections.
Dr Nazirah Hasnan, deputy medical director and co-chair of the Covid-19 task force at Universiti Malaya Medical Centre (UMMC), and Dr Marzuki Isahak — who is a UMMC public health specialist and occupational safety and health expert — expressed certainty that health care workers (HCW) in Covid-19 wards at UMMC are safe from infection, if they follow all recommendations on personal protective equipment (PPE) use and patient handling guidelines.
Dr Nazirah and Dr Marzuki also shared that the UMMC Department of Occupational Safety and Health together with the Department of Public Health have joined forces to form the HCW Surveillance team, reporting to the Covid-19 Task Force and Management. This task force allows for better contact tracing, risk assessment, and patient surveillance at UMMC, a public university hospital here that manages and treats coronavirus patients.
“All HCW have to follow all the procedures to ensure theirs and their co-workers’ safety as well as patient safety. All HCW in contact with suspected and positive Covid patients will be traced, risk assessed and investigated,” Dr Nazirah and Dr Marzuki told CodeBlue in an interview.
“HCW with symptoms will undergo clinical examination and (be) managed accordingly, even without exposure history.
“With the current available evidence and the strict surveillance and risk assessment system in the hospital, we do not perform mass testing for all HCW, but targeted and risk-based testing,” they added.

Dr Victor Hoe, a professor of occupational and public health at Universiti Malaya, said UMMC uses an online symptom-checking tool. Health workers must complete that assessment before they report to work. A similar symptom check list is also being developed for all patients and visitors of the university hospital.
“From our experience and the data from the Ministry of Health Malaysia, we are confident with the control measures that we are taking in the hospital, HCW will not be at risk of getting infection while attending to a patient if the HCW has followed the recommended procedure,” Dr Hoe told CodeBlue.
Five Covid-19 clusters have broken out at various Ministry of Health (MOH) facilities, such as Sarawak General Hospital (SGH) in Kuching with 68 cases among HCW; 35 cases among Sabah health care workers in Kota Kinabalu, Penampang, Keningau and Tuaran; 24 infections in Muar Hospital, Johor; 16 cases among Sungai Buloh health care workers in Selangor; as well as the previous case of 37 infected health care workers at Teluk Intan Hospital in Perak.
While HCW from other hospitals have been quiet, some SGH staff have criticised the allegedly poor quarantine and infection control procedures at their institution, such as a frustrated SGH health care worker who sent a letter to CodeBlue, complaining about hospital policies changing every day. Dr Nazirah and Dr Hoe were asked to comment on this issue.
“I can’t comment on other hospitals’ practices. But I’m not surprised that there are changes in policies etc, as we have new knowledge, evidence and international updates,” said Dr Nazirah.
“The whole world is learning about Covid-19 and everyone and every institution will continuously update their guidelines and policies according to new and current evidence.”
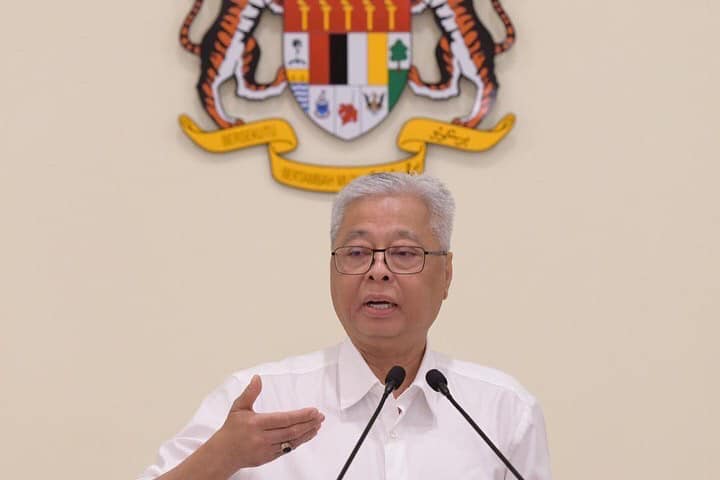
Dr Nazirah Hasnan, deputy medical director and co-chair of the Covid-19 task force at Universiti Malaya Medical Centre (UMMC)
Dr Hoe cited MOH’s Covid-19 guideline that is currently in its 5th edition and available on the MOH website, and noted that these guidelines are adopted and adapted to fit UMMC’s requirements.
“Quarantine procedures are all based on the risk of exposure of the health care workers, and all quarantine goes through the District Health Office, as only the District Health Officer (Medical Officer of Health) has the authority to issue quarantine notice.
“For workers who are at High Risk of exposure, a 14-day quarantine notice will be issued, Medium Risk of Exposure — a seven-day quarantine notice, Low Risk of exposure — two days (of Medical Certificate) MC until the results of the test, and No-Risk of Exposure (would be given) no test and no leave. The risk of exposure is based on all risk of exposures, (for example), work and non-work,” he explained.
How To Define Hospital-Acquired Infections

Earlier last month, public confusion with infection terminology arose from MOH’s reports on its health care workers who tested positive for Covid-19, where Health director-general Dr Noor Hisham emphasised that none of the cases involved handling coronavirus patients in the Covid-19 or intensive care unit (ICU) wards.
In a letter to CodeBlue, paediatricians Dr Musa Mohd Nordin and Dr Zulkifli Ismail expressed their view that if Covid-19 was acquired within hospital facilities, whether in the pantry or from co-workers, it should be classified as a hospital-acquired infection (HAI).
In that light, Dr Hoe explained that MOH referred to those positive Covid-19 cases among HCW as occupational disease, not hospital-acquired infection.
“The reason the Director-General of Health specifically pointed out that none of the HCW that is Covid-19 positive acquired it from a Covid-19 patient is to reassure the HCW and the public that the control measures that we are implementing in hospitals are appropriate and adequate,” said Dr Hoe.
“We want to ensure that HCW are confident in the control measure and can work without feeling afraid or scared.”
Dr Victor Hoe, professor of occupational and public health at Universiti Malaya
“Occupational disease has a specific definition under the Occupational Safety and Health Act 1994 (OSHA 1994). It is an infection acquired in the course of doing the job in the workplace. This means the health care workers’ job of managing the patient in the hospital or clinic settings.
“Hospital-acquired or nosocomial infection, on the other hand, is usually reserved for patients who acquired the infection from the hospital,” he explained.
Dr Hoe also further added that the OSHA 1994 and Employees Social Security Act 1969 both state that only diseases acquired in the course of the job are classified as occupational diseases.
“If a worker acquired the infection from another worker, it is not considered as an occupational disease, it is considered as a community-acquired disease. The only difference is the community is now in the hospital or workplace,” explained Dr Hoe.
“This is important, if not every time anyone gets a flu or cough from their colleague, we will consider it as occupation disease.”

Echoing Dr Hoe’s clarification, Dr Nazirah and Dr Marzuki provided an example to better explain the different terminology pertaining to the source of infection:
“(A Covid-19) positive HCW in contact with Covid-19 patients in non-Covid-19 wards or clinics or emergency departments, before (those patients) are being diagnosed as Covid-19 (positive), is still considered as work-related infection.”
According to the World Health Organization’s (WHO) definitions, an “occupational disease” is any disease contracted primarily as a result of an exposure to risk factors arising from work activity, whereas “work-related diseases” have multiple causes, where factors in the work environment may play a role, together with other risk factors, in the development of such diseases.
WHO’s definition of hospital-acquired infection (HAI) or health care-associated infection, also referred to as “nosocomial” or “hospital” infection, is an infection occurring in a patient during the process of care in a hospital or other health care facility which was not present at the time of admission.
Companies Must Identify High-Risk Jobs And Areas, Appoint Safety Officers

As the nation enters its second phase of Conditional Movement Control Order (CMCO) from today to June 9, many more would be returning to work in order to restart the country’s economy. However, Malaysians would now have to adhere to a “new normal” in their daily living, including possible exposure to the coronavirus in the community.
“For the risk of the workers spreading the disease (in) the workplace, the companies need to identify high-risk jobs. This includes jobs with exposure to the public, for example receptions, guards, delivery personnel, sales personnel, etc.
“They also need to identify areas in the company where there is high traffic flow and where many workers need to gather. After identification of the risk, appropriate training for the workers and control measures need to be implemented in those areas,” said Dr Hoe, when asked to give advice to companies that are reopening post-MCO.
Dr Nazirah and Dr Marzuki added that for companies to ensure that all employees adhere to standard operating procedures (SOP) on safe distancing and other health measures, they would have to appoint a safety officer or representative in the company to enforce the SOP properly.
“Giving the mask does not mean the employer has transferred the responsibility to the employees. Employers need to monitor all employees and make sure that the employees comply with the recommendation,” said Dr Nazirah and Dr Marzuki.
“Companies must have adequate policies to ensure that ‘trust’ is built. Maintaining confidentiality and minimising stigma are key components.
“Apart from avoiding misconceptions, misinformation, and rumours through health promotion, companies will have to build collective solidarity, where a worker is required to self-quarantine. Leave policies and pay policies must be ensured to be fair,” they added.
Universiti Malaya recently developed a guideline titled “Return to work after the Movement Control Order (MCO) for Covid-19 Infection – A Guide for Workplace” on how workplaces can prepare to reopen post-MCO.
Unnecessary To Shutter Company With One Infected Worker
Senior Defence Minister Ismail Sabri Yaakob previously said in a press conference that if one employee tests positive for Covid-19, the company will be shut down. But Dr Hoe, Dr Nazirah, and Dr Marzuki all disagreed with this method, stating that it is unnecessary to close an entire corporation.
“We would have to shut down the entire hospital then if that advice is taken into consideration. That single infected worker might not have been in contact with all the workers and working area,” said Dr Nazirah and Dr Marzuki.
Dr Hoe said the government shouldn’t put “fear” into companies, but should instead assist them to develop policies and control measures for the “new norm” during the Covid-19 pandemic.
“A punitive action will be counterproductive,” he said.
“In the new norm, business cannot be as usual. Health of the workers should be considered an important asset for the company. The responsibility for maintaining health of the workers should be a shared responsibility between the employer, workers and health care providers.”








