KUALA LUMPUR, April 17 — An epidemiologist has supported the Ministry of Health’s (MOH) strategy of doing targeted instead of mass testing for Covid-19 in a middle-income country like Malaysia.
Dr Nirmala Bhoo Pathy, a public health medicine specialist and associate professor of epidemiology at Universiti Malaya, said most people would simply have mild coronavirus infection and that mass testing was a waste of resources.
“If you test everybody, what are you going to do with them? Are you going to put them in a facility?” Dr Nirmala told CodeBlue in an interview.
“What we’re doing now is good — identify high-risk people and once you identify a group, identify a cluster, test all. This is what I think is the best approach for our country.
“You cannot follow WHO (World Health Organization) ‘test, test, test’. I’m definitely not a proponent of test, test, test for everyone. What MOH is doing is the correct thing, given our resources. You must always test based on what you have.”
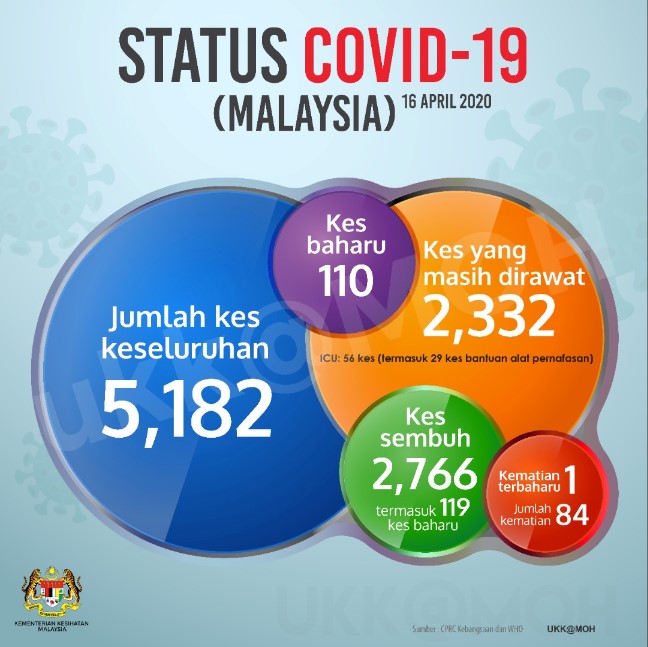
MOH has recently started pushing out data on the number of active infectious cases in the country, a figure derived from deducting recoveries and fatalities from the total number of confirmed Covid-19 infections. Health authorities reported 2,332 active infectious cases as of yesterday.
Dr Nirmala explained that active infectious cases were really cases of moderate to severe coronavirus infection.
“The ones who are mild are never going to be in the picture because we never tested them to identify them in the first place.”
When asked if there was a possibility of people with mild infections or who do not show symptoms yet unknowingly infecting others who were more likely to develop severe illness, Dr Nirmala acknowledged that this risk existed.
“But when we target red zones and try to get clusters, identify far-reaching areas where clusters have spread, at least what we’re doing is reducing the probability that a presymptomatic person is infecting a vulnerable person,” she responded.
Health director-general Dr Noor Hisham Abdullah said yesterday that MOH has ordered a South Korean antigen rapid test kit, of which samples can be taken at clinics or hospitals and do not have to be sent to Malaysia’s 43 laboratories. MOH hopes to use these to increase testing in targeted populations and locations. Antigens are viral proteins expressed only when the virus is actively replicating, so tests based on antigen detection can identify acute or early infection, according to WHO.
The high-risk groups or locations targeted by health authorities for testing are the current 28 coronavirus clusters in Malaysia, or those related to the tabligh gathering at Sri Petaling mosque last month that accounts for 40 per cent of cases. MOH will also look into testing residents at aged care facilities, as Covid-19 incidence is highest among those aged 55 to 69.
When asked if antibody rapid test kits — with results in minutes compared to typical PCR test results that can take 24 to 48 hours — could be used to look at the true pattern of the epidemic, Dr Nirmala said this could be done if research funding was available. Antibodies take days to weeks to develop after a viral infection; as such, antibody tests can’t be used for Covid-19 diagnosis, but may be useful in disease surveillance and epidemiological research.
“If we can get money and funding, you have an area where you have one hospital, it would be nice for our knowledge to know what was the real rate,” she said. “But that is ideal lah.”
How Is Malaysia Faring?
Dr Nirmala believed that deaths per million population and the case fatality rate (the number of deaths over the number of cases) were better measures of Malaysia’s success in tackling the Covid-19 outbreak when comparing to other countries, rather than the absolute number of deaths or the number of cases.
Comparing the number of coronavirus-related deaths between Malaysia and other countries is influenced by how healthy a population is. Malaysia, she said, has many young people, compared to European nations with an older population that also suffer from underlying illnesses. Old age and pre-existing conditions are more likely to lead to severe disease from Covid-19.
Eighty-four people have died from Covid-19 in Malaysia as of yesterday. Countries like the United States, Italy, Spain, France, and the United Kingdom, however, have recorded over 10,000 deaths.
As for comparing the number of Covid-19 infections between countries, this is essentially comparing testing rates, said Dr Nirmala. Malaysia reported 5,182 coronavirus cases as of yesterday.
“That’s why I like deaths per million population. When you do that, you cancel the age and effect of comorbidities. So in that sense, when you want to do international benchmarking, I think that’s a better measure.”
Dr Nirmala Bhoo Pathy, associate professor of epidemiology from Universiti Malaya
Malaysia has three Covid-19 deaths per million population, same as in the Philippines, compared to two in Singapore. South Korea recorded four deaths per million population, while Australia reported two. Spain reported the third highest deaths per million population in the world at 402, while Italy recorded 358 deaths per million population, the UK (190), and the US (86).
The mortality or case fatality rate, meanwhile, depends on the number of cases. So, a country like Australia could have a low case fatality rate if it captures mild cases in mass testing. Australia’s coronavirus mortality rate is less than 1 per cent, compared to Malaysia’s 1.6 per cent. South Korea’s Covid-19 mortality rate is about 2.2 per cent, while the US records a 4.4 per cent case fatality rate. The coronavirus mortality rates are about 13.1 per cent in Italy and 10.4 per cent in Spain.
But the case fatality rate, said Dr Nirmala, would be more useful than tracking mortality per million population in under-resourced countries like Indonesia and India that may not be able to track all births and deaths in their large populations. Indonesia’s Covid-19 case fatality rate is about 9 per cent.
“I think we’re doing not bad at all. In my heart, I feel very contented because most of our actions are heading the right way,” she said.
“If everybody does their part, we’re sure heading to success. My fear is the Movement Control Order (MCO) is going to end, and even now, people are misbehaving. So if we have people misbehaving, our efforts are going to be wasted.”
Besides international benchmarking, Malaysia can also do internal comparisons by looking at the Covid-19 epidemic over time, such as measuring the time taken for the number of cases to double, with the caveat that testing policies remain consistent, said Dr Nirmala.
Malaysia reported 428 confirmed cases as of March 15. This doubled to 900 cases in four days by March 19. Covid-19 infections then doubled to about 1,800 in six days by March 25. It took 11 days for cases to double to about 3,600 by April 5.
“The time is increasing, which means it’s good,” she said.
When asked if Malaysia has passed the Covid-19 peak, Dr Nirmala said it was still too early to tell, but the epidemiological curve may flatten if there is a pattern of declining cases and deaths.
“If we’re seeing everything reducing, then we can be sure we’re doing the right thing,” the epidemiologist said. “I feel that we’re headed the right path.”
Post-MCO Measures

When asked if the current data was sufficient to begin planning for reopening the country after April 28, the end-date of the third phase of the MCO, Dr Nirmala said epidemiological models were mostly based on assumptions that could be undone by unpredictable human behaviour. Malaysia also is still uncertain about the number of people with mild coronavirus infection.
The epidemiologist suggested that Malaysia look at historical studies in the US on the Spanish flu that test the duration of various forms of lockdown.
“That shows the longer you sustain those things, the better, but it may not necessarily be a full-fledged MCO,” she said, suggesting measures like keeping schools and educational institutions closed, banning mass gatherings, and limiting international travel.
The migrant community must also be taken into account as public health concerns all residents.
“This MCO has provided training for the Malaysian population,” she said. “People have to realise, when the MCO is lifted, it’s not business as usual. It’s a new normal. We have to train our people to accept the new normal.”
As for what kind of businesses should reopen after the nationwide partial lockdown ends, Dr Nirmala urged the government not to take a top-down approach, but to work out solutions together with businesses that would know the situation best on the ground.
“I think we should encourage and call all the bright minds in the private sector and come up with solutions together. That’s how we’re going to deal with it.”








