KUALA LUMPUR, Sept 8 – ProtectHealth Corporation has shockingly told Madani Medical Scheme (SPM) panel clinics to change treatment plans for cost containment if treatment costs exceed patients’ benefit limits – and to subsequently refer patients to the public sector.
The maximum limits reimbursable for private general practitioner (GP) clinics empanelled under SPM – as set by the company fully owned by the Ministry of Health (MOH) – are as follows, per patient visit: RM60 for combined consultation and medication, RM50 for investigations (point-of-care testing or diagnostic procedures), and RM50 for therapeutic procedures.
“If you encounter a scenario in which a patient’s treatment costs exceed the maximum limit, our suggestion is to modify the treatment plan so that it aligns with the per-claim constraints, and subsequently, to refer the patient to a government facility for further care,” ProtectHealth said in an email yesterday to SPM panel clinics, as sighted by CodeBlue.
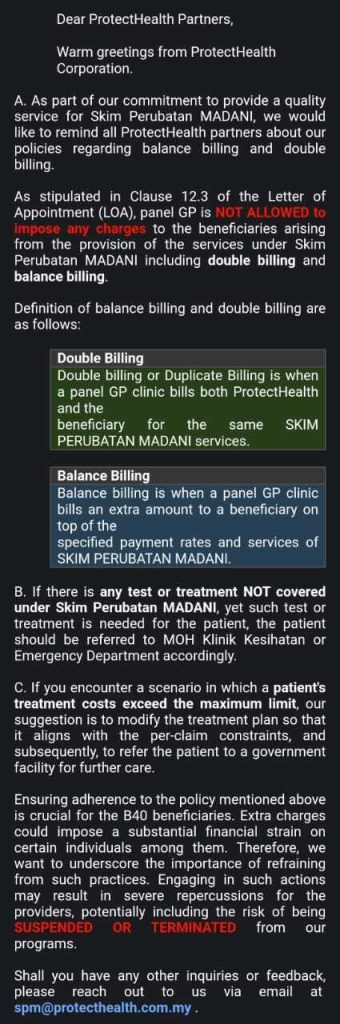
ProtectHealth also reminded panel GP clinics not to charge patients under the SPM programme, including double billing and balance billing, as stipulated in their letter of appointment with the company.
Double billing is defined as billing both ProtectHealth and the beneficiary for the same SPM services, whereas balance billing occurs when a panel clinic bills an extra amount to a beneficiary on top of the specified payment rates and services of SPM.
ProtectHealth further told panel clinics to refer patients to public health clinics or emergency departments under the MOH if needed tests or treatments were not covered under SPM.
“Ensuring adherence to the policy mentioned above is crucial for the B40 beneficiaries. Extra charges could impose a substantial financial strain on certain individuals among them.
“Therefore, we want to underscore the importance of refraining from such practices. Engaging in such actions may result in severe repercussions for the providers, potentially including the risk of being SUSPENDED OR TERMINATED from our programs.”
ProtectHealth’s website on SPM did not inform low-income beneficiaries about the maximum limits per visit for combined consultation and medication (RM60), investigations (RM50), or therapeutic procedures (RM50), merely stating that the overall benefit limits for treatment of acute conditions, until year-end, are RM250 for households, RM125 for senior citizens, and RM75 for singles.
In an FAQ, the company simply stated on its website – in response to a question on action required if the treatment package charged by GPs exceeded one’s visit entitlement limit under SPM – that GPs are “prohibited from imposing additional charges”.
ProtectHealth’s email to SPM panel clinics yesterday was sent, despite Health Minister Dr Zaliha Mustafa announcing just two days prior that the government was reviewing reimbursable fees for GPs under the programme.
This followed complaints from doctors’ groups about the fees and price list – as low as 93 per cent below market rates – for consultation and various medications, investigations, and basic therapeutic procedures. The maximum consultation rate under SPM is RM30; doctors’ groups have asked for RM50.
Modifying Treatment Plan Suggestion Interferes With Doctors’ Autonomy, Raises Malpractice Potential

Federation of Private Medical Practitioners’ Associations, Malaysia (FPMPAM) president Dr Shanmuganathan Ganeson slammed ProtectHealth’s suggestion of modifying treatment plans to stay within a patient’s benefit limits as “interference in doctors’ autonomy”.
“In all instances, the doctor in a managed care system has to place the interests of the patient and confidentiality above all other considerations,” he told CodeBlue.
“He should refrain from entering into a contract with a managed care organisation if there are potential areas of ethical conflict in his professional autonomy and doctor-patient relationship,” he added, citing stipulations of such contracts in the Private Healthcare Facilities and Services Act 1998.
Dr Saravanan Ramasamy, an SPM panel GP who practises in Shah Alam, Selangor, told CodeBlue that the potential for malpractice suits arising from the need to modify treatment plans to contain costs was “low, at least for now”.
He explained that this was due to low literacy levels among the B40 group and the 20 per cent of SPM patients from the middle class (M40), in his experience, who mostly come to the clinic either for medical leave or to “just collect medicine for common illnesses”.
“But there is definitely room for improvement as far as the quality of care rendered to patients is concerned. This can be achieved with a simple restructuring of the per-visit price limit and by respecting personal autonomy – allowing patients to pay for their health care if they choose to do so. At present, this scheme puts both patients and doctors between a rock and a hard place.”
When asked if he expected SPM panel clinics to modify treatment plans or refer patients to government clinics due to the low benefit limit of RM60 per visit, Dr Saravanan stressed that most GP clinics were solo practitioners operating with high overheads and “an almost moderate income”.
He also claimed that labs and pharmacies are conducting their own medical consultations and managing illnesses with “almost no enforcement mechanism put in place against them”.
“As such, we can only afford that much of goodwill and charity. Though we are bearers of the Hippocratic Oath, we too have mouths to feed and bills to pay. I am quite confident that most, if not all, my fellow GPs will try their best to help treat and provide the best of care to their patients.
“I hope ProtectHealth realises this and upgrades its payment limits before it becomes the straw that breaks the camel’s back. I personally don’t see GPs mass referring patients to other public health care clinics should this happen. Instead, fatigue will set in and many will pull out of the programme.”
Medical Practitioners Coalition Association of Malaysia (MPCAM) president Dr Soo Tai Kang said while he agreed with ProtectHealth’s policy against double billing, the company’s “tight control of the charges will eventually change the practice of the doctor”.
“In a case of the alteration of practice causing direct or indirect harm to the patient, it is malpractice – even in mild trauma or surgical-indicated”.
The similar Skim Peduli Sihat (SPS) programme by the Selangor state government, which is nearly seven years old, had a much higher allocation of RM125 million during its December 2016 launch, compared to RM100 million for the nationwide SPM launched last June. SPS benefit limits are higher than SPM at RM500 for households and RM200 for singles annually, with an RM70 limit per treatment for basic health treatment (including vaccination) at panel clinics.








