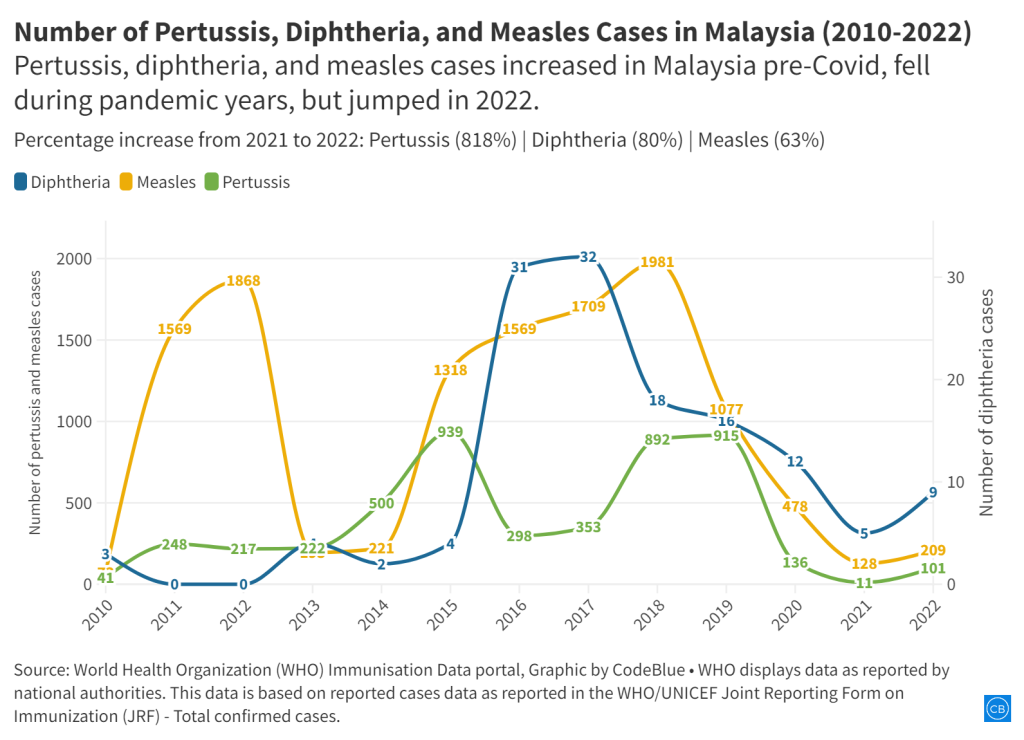
KUALA LUMPUR, August 22 — Cases of vaccine-preventable childhood diseases – pertussis (whooping cough), diphtheria, and measles – jumped in Malaysia last year post-Covid pandemic
According to data published last July by the World Health Organization (WHO) and Unicef on global childhood immunisation recovery after historic backsliding caused by the Covid-19 pandemic, Malaysia reported a spike in cases of all three infectious diseases in 2022.
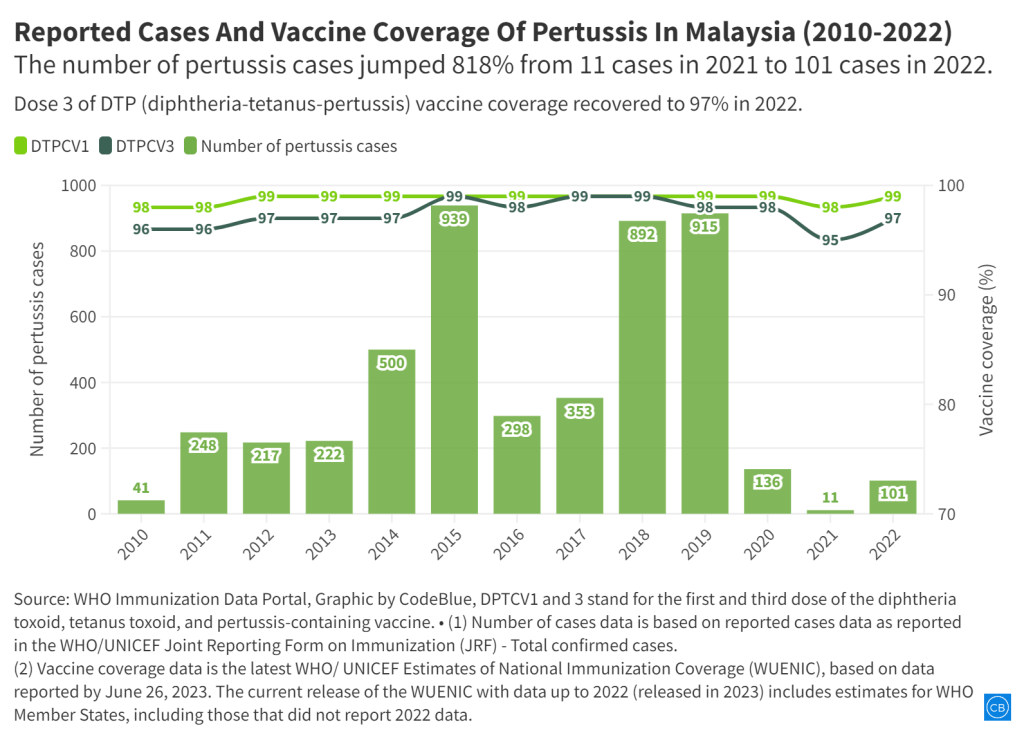
Nationwide, pertussis cases leapt 818 per cent last year to 101 cases from the 11 cases recorded in 2021.
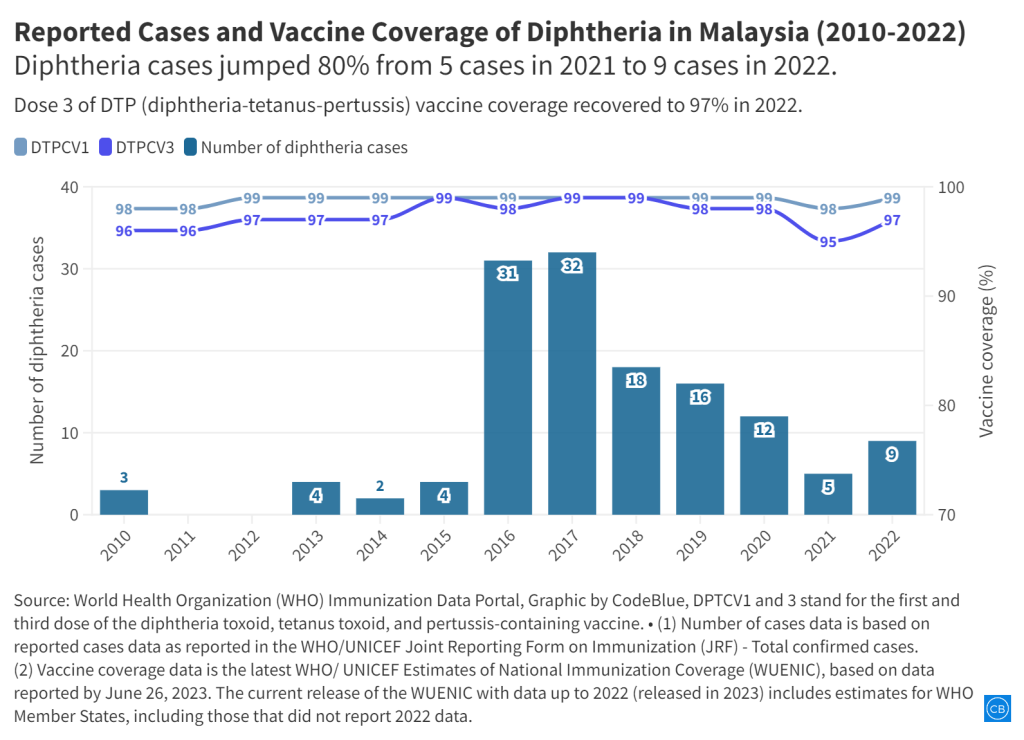
Diphtheria was the second disease to see a significant jump in numbers from five cases in 2021 to nine cases in 2022, marking an 80 per cent rise.
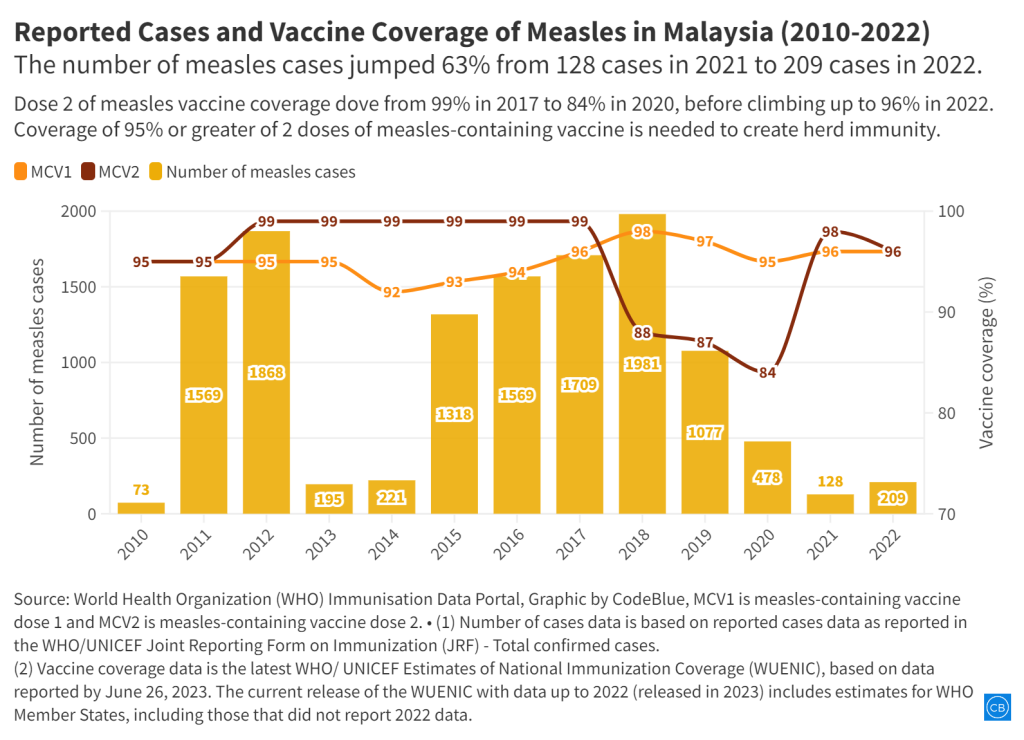
Finally, measles cases rose 63 per cent in 2022, recording 209 cases for the year from 128 cases in 2021.
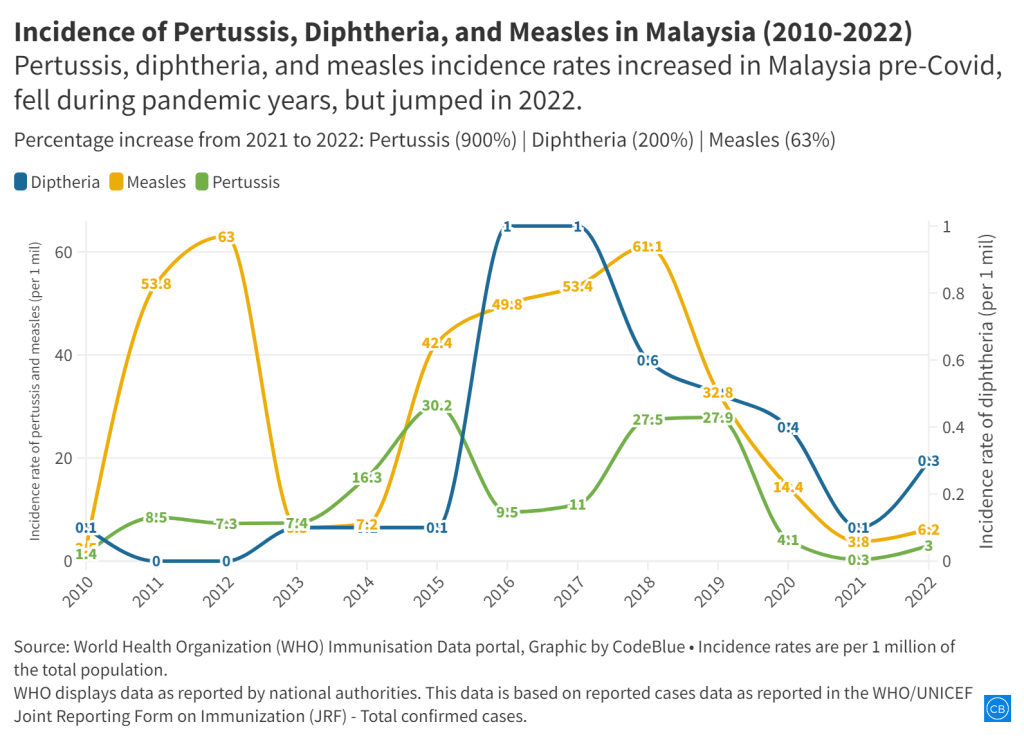
Since 2015, measles recorded the highest incidence rates among the three infectious diseases. Last year, the incidence rate for measles was reported at 6.2 cases per one million total population, compared to three cases per million population for pertussis and 0.3 cases per million population for diphtheria.
The reported rise in pertussis, diphtheria, and measles cases in Malaysia in 2022 was the first increase since steep declines from 2020 for pertussis, 2019 for measles, and 2018 for diphtheria.
Even though immunisation coverage with the first and third dose of the diphtheria-tetanus-pertussis vaccine remained above 95 per cent in Malaysia for more than a decade since 2010, cases of pertussis and diphtheria fluctuated throughout that period.
The data for measles is also puzzling. Measles cases spiked 496 per cent from 221 cases in 2014 to 1,318 cases in 2015, climbing steadily in subsequent years to nearly 2,000 in 2018, before a 46 per cent decline to 1,077 cases in 2019. Cases further fell to 128 in 2021, before a 63 per cent rise to 209 last year.
From 2013 to 2014, immunisation coverage with the first dose of the measles vaccine dropped from 95 per cent to 92 per cent, before climbing steadily in subsequent years to hit 98 per cent in 2018. Dose Two coverage fell from 99 per cent in 2017 to 84 per cent in 2020, before climbing back up to 98 per cent in 2021 during the Covid-19 pandemic and dipping slightly to 96 per cent in 2022.
The Pahang state health department reported last Friday a pertussis outbreak of three cases in a family in Kampung Bahagia, Rompin, involving two children and their mother. Pahang state health director Dr Nor Azimi Yunus urged parents to get their children completely vaccinated against pertussis at ages two, three, five, and 18 months.
According to 2010 guidelines by the MOH’s disease control division for health care personnel on pertussis, an outbreak is defined as two or more cases clustered in time (occurring within 42 days of each other) and space.
Pertussis, diphtheria, and measles are vaccine-preventable childhood diseases that can cause serious and sometimes deadly complications.
To explain the puzzling rise in pertussis, diphtheria, and measles despite high vaccination rates over the past decade or so, CodeBlue interviewed three paediatricians: Dr Zulkifli Ismail, Dr Musa Mohd Nordin and Dr Amar-Singh HSS.
To view the jpeg graphics of the charts, scroll to the bottom of the article.
Dr Zulkifli Ismail: Minute Vaccination Drop Disrupted Herd Immunity

Dr Zulkifli Ismail, consultant paediatrician and paediatric cardiologist at KPJ Selangor Specialist Hospital, explained that the dip in childhood vaccination rates during the Covid-19 pandemic was enough to disrupt herd immunity, while cases fell at that time due to lockdowns.
“During the pandemic in 2021, there were drops in the vaccine uptake of DTP (diphtheria, tetanus and pertussis) and MMR (measles, mumps and rubella) due to various reasons, one of which was the movement control orders. At the same time, childcare centres and public places were closed. There was no spread of the infections.
“The small drop in vaccination rates in 2020 and 2021 (worldwide) was enough to disrupt herd immunity. This makes a segment of the population vulnerable to pertussis and measles.
“As the pathogens are still circulating among infected and carriers, the opening of child care centres and public gatherings just allows the spread to the unvaccinated and those too young to receive the vaccines,” Dr Zulkifli said in a written response to CodeBlue.
The chairman of the Immunise4Life (IFL) programme held that the diminishing uptake in vaccinations – such as the DTP and MMR vaccines – could be attributed in part to the fear surrounding Covid vaccinations, as the public “has started to lump together all vaccines”.
Dr Zulkifli said this was a “dangerous trend because vaccine refusal increased from an average of one to two per thousand live births to 3.2 in 2021.”
According to Dr Zulkifli, the rise in measles cases last year was a delayed reaction to the poor uptake of the MMR vaccine in the years before the Covid-19 pandemic.
“There is usually a slight lag between the drop in uptake and the spike of cases,” he explained.
“The MMR vaccine has been the target of anti-vaccine movements over the years. The fraudulent link of MMR vaccine with autism has been drummed up over and over again despite the fact that Andrew Wakefield’s paper was retracted by the journals and refuted by his co-authors. This controversy has caused the irregular uptake of the MMR vaccine.”
Parent absentmindedness is yet another reason for the drop in vaccination rates, according to Dr Zulkifli.
“The MMR vaccine is also given at one-year-old before (and recently at nine months and one year). These are the ages when parents occasionally forget to take their children for vaccination.
“Malaysia has been trying to achieve measles elimination and the deadline has been deferred many times. I think the current target is 2024 but looking at the data, it is not possible to achieve 1 case per million population for three consecutive years without near 100 per cent MMR vaccination coverage.”
Last year, the incidence rate for measles was 6.2 cases per million population.
Dr Musa Mohd Nordin: Granular Data Needed for Measles

Primary and secondary vaccine failures due to early vaccinations and waning immunity are two reasons for measles outbreaks, said Dr Musa Mohd Nordin, a paediatrician who sub-specialises in neonatology at KPJ Damansara Specialist Hospital.
“Primary vaccine failure – five per cent do not seroconvert and develop protective antibodies, and this failure is higher if the MCV (measles-containing vaccine) is administered before the child is one year old, due to circulating maternal antibodies in the child.
“Thus, why two doses of the MCV vaccine is recommended.
“Secondary vaccine failure due to waning immunity, which may occur in two to 10 per cent of vaccinees.”
Under Malaysia’s National Immunisation Programme (NIP), the first dose of the MMR vaccine is administered when the child is nine months old; the second dose is administered at 12 months.
Dr Musa held that vaccine failures are generally associated with milder diseases, such as modified measles, since vaccination mitigates measles complications.
“Since vaccination mitigates measles complications with lowered incidence of measles due to vaccination, there is reduced natural exposure in childhood, and thus, less natural boosting,” said Dr Musa in a written response to CodeBlue.
Suboptimal vaccine coverage, according to Dr Musa, has also led to measles outbreaks, which would be significantly reduced if vaccination rates for the second dose of the MCV vaccine was above 95 per cent, conferring herd immunity.
According to Dr Musa, granular data on the 209 reported measles cases in Malaysia last year would be very insightful.
To illustrate his point, Dr Musa shared Ministry of Health (MOH) granular data for the 2017 and 2018 measles outbreaks that saw 1,693 and 1,934 cases respectively (these are slightly lower than WHO data of 1,709 and 1,981 cases respectively).
In 2017, about 28 per cent of the measles cases recorded by the MOH were vaccinated, 31 per cent were not vaccinated, 23 per cent were not eligible for vaccination, and 18 per cent were of unknown status.
In 2018, about 24 per cent were vaccinated, 33 per cent were unvaccinated, 25 per cent were eligible for vaccination and 18 per cent were of unknown status.
On pertussis specifically, Dr Musa said that having data on the age of the person who contracted whooping cough would aid in determining the next appropriate public health intervention.
“For pertussis, apart from vaccination status, it would be helpful to know the age of the pertussis cases.
“During the period 2012 to 2018, there were 55 deaths (based on MOH data) due to pertussis – the highest being 22 in 2018. Nineteen (86 per cent) of the deaths were in infants less than six months old.
“Thus, the current initiative to vaccinate pregnant women with Tdap (tetanus, diphtheria and pertussis vaccine) to prevent pertussis, neonatal tetanus and diphtheria during this most vulnerable early infancy period.”
Dr Amar-Singh HSS: Post-Pandemic Rise In Childhood Infectious Disease Natural

Consultant paediatrician Dr Amar-Singh HSS opined that the opening of schools and preschools post-pandemic would naturally lead to an increase of cases of childhood infectious disease.
He projected that the number of measles, pertussis, and diphtheria cases would rise even higher for the second half of this year, as societal mask mandates are dropped.
“What we need to do is to compare average pre-pandemic rates with post-pandemic rates (once a return to routine activities was established) to really be certain that the rise in measles, pertussis, and diphtheria cases seen in 2022 is significant,” Dr Amar told CodeBlue.
Additionally, the consultant paediatrician advocated for disaggregated data from the MOH “to have a meaningful interpretation of the data.”
Dr Amar said the MOH data needs to provide answers to the following questions:
- Have children who missed their primary vaccination in the 2020 to 2022 period been vaccinated (i.e. catch-up vaccination)? If they have not, they then pose as an unvaccinated cohort that impairs herd immunity.
- Are those who are currently infected with measles, pertussis and diphtheria vaccinated or do they belong to the vaccine hesitancy (refusal) group? We are aware from data that some of those who choose not to vaccinate their children live in religious communities. This enables the rapid spread of communicable diseases in unvaccinated children.
- Which geographical region in the country are the children living in who were infected with measles, pertussis and diphtheria in 2022? Are they stateless children, documented and undocumented migrants? We are aware that there are many stateless and undocumented migrants in Sabah and the Klang Valley. Have we taken steps to provide their children free access to primary vaccination? If we do not do this, we harm the herd immunity of Malaysian children.
- How good is the vaccine cold chain in the public and private sectors to ensure the delivery of quality vaccines? Prior studies show significant weaknesses in both the private and public sectors. Has any recent assessment been conducted to ensure that the vaccine cold chain is maintained?
On pertussis, in particular, Dr Amar held it is not clinically easy to diagnose the disease, leading to the fluctuations in pertussis data over the past two decades.
Therefore, he was of the opinion that using pertussis rates to “monitor any impact of programmes or measures is of little value”.
“Overall, the current increase in measles, pertussis and diphtheria rates is small, compared to pre-pandemic numbers, but it is an indicator that they will rise further in 2023. It would be prudent to take concerted steps to halt a significant rise”.