KUALA LUMPUR, Feb 23 – The Malaysian Medical Association (MMA) has proposed a 178 per cent increase in doctors’ weekend on-call claims to RM25 per hour from the current hourly RM9 rate.
In an audio recording obtained by CodeBlue, members of the doctors’ group were heard briefing Health Minister Dr Zaliha Mustafa during her town hall session with government doctors yesterday on a number of issues in the increasingly strained public health service.
These included low on-call claims and salaries, bullying, unclear criteria for permanent positions, unrecognised years of service under the contract system, last-minute placement instructions, expensive subspecialty training, and poor hospital facilities, among other problems.
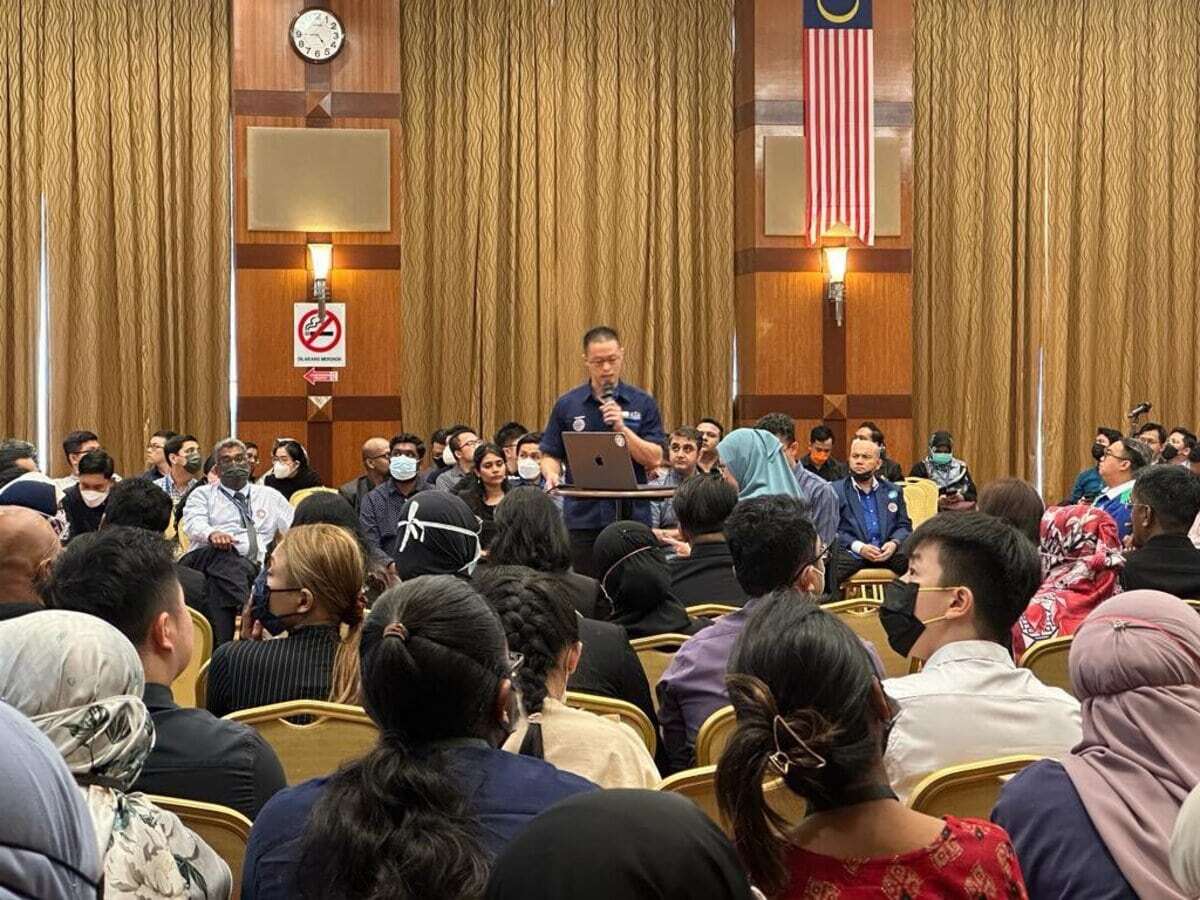
MMA was co-organiser, along with the Ministry of Health (MOH), of the closed-door meeting held under the Chatham House Rule at the ministry’s headquarters in Putrajaya with some 300 junior and senior medical doctors from the public sector.
During the town hall, a participant compared Malaysia’s on-call claim rate against Singapore’s on-call rate and other part-time roles in the services sector.
“I think it has been 10 years since our on-call claim was increased. This is just to give a rough comparison as to how much we are paying certain retail workers, about RM10 per hour for certain baristas from certain coffee companies, our cleaners are paid RM20 an hour – and the comparison (RM9 per hour on-call weekend rate in Malaysia).
“Friends across the Causeway get paid about RM60 per hour for on-calls. RM10 (per hour for retail sales assistant), RM10 (per hour for baristas), RM20 (per hour for house cleaners), and that’s (RM9 per hour) our on-call claim here.
“Some would say, wait, ini ialah elaun on-call, bukan gaji (this is on-call allowance, not salary). Let’s look at salaries. Salary [for housemen] is about RM5,000 for about 300 hours of work a month. It also comes to about RM16 an hour, which is still less than your friendly cleaner lady,” the doctor said.
Despite pushing for a substantial increase, MMA’s proposal to raise doctors’ on-call rate to RM25 per hour would still be less than half of what doctors in Singapore receive for their on-call duties. “This is obviously something that is not achievable overnight, I understand. But it’s a proposal.”
Bullying: Everything Everywhere All At Once
The issue of bullying was raised by a town hall participant, who said that the dynamics have become more complicated and now involves professionals at all levels, not just specialists against medical officers or housemen.
“[It’s happening] among specialists to consultants, matrons towards sisters, sisters towards nurses, nurses towards housemen, housemen towards medical officers, housemen towards medical students also.
“So it goes up and down the ladder, everywhere.”
Referring to the tragic incident of a house officer’s death in Penang last year, the doctor said that bullying in the medical profession can manifest as snide comments from senior officers.
“All of a sudden there were many experts, many snide remarks. Many specialists, when they want to marah during rounds, they will say, ‘tak nak marah lah, nanti dia terjun dari tingkap.’ Such remarks like that were very, very common,” the doctor said.
Also present during the town hall session was Deputy Health Minister Lukanisman Awang Sauni and government backbenchers from the DAP, Bandar Kuching MP Dr Kelvin Yii and Ipoh Timor MP Howard Lee Chuan How. Dr Helmy Haja Mydin, who is special advisor to the health minister, moderated the meeting.
“The ministry does suggest that those who are affected to launch SISPAA (Sistem Pengurusan Aduan Awam). However, there are many ‘dinosaurs’ in the system who are collecting SISPAA complaints like collecting designer bags,” the doctor said.
“We may have the best health care system, but we clearly do not have the healthiest health care environment. So, please help us put an end to this.”
Unclear Selection Criteria, Fixed Pay Grades In Contract System
Although doctors appreciated the previous government’s efforts to provide over 4,000 permanent positions for medical, dental, and pharmacy officers in the past year, they maintained that the lack of clear selection criteria for these positions is a persistent issue.
A town hall participant stated that the MMA has developed a point-based system for selecting candidates for permanent positions and is planning to share the draft with MOH in the near future.
Pay grade was another issue that was brought up in relation to the contract system.
“Since the contract system is in place, the first contract that a houseman gets is a three-year contract as a UD41. And housemen, if they don’t get any extension, they can finish their housemanship in two years.
“But during that one year as a medical officer, they are still under UD41, which we feel is not setara. As medical officers, they have a lot more responsibilities and yet, they are still UD41,” the doctor said.
“Our suggestion is that, if possible, once they finish the housemanship, they can go straight to UD43, even before the end of their three-year contract.”
Another concern raised is that the years of service rendered under a contract are not taken into account when they join permanent service, as highlighted by an example of an officer who served four years under contract and two years as a permanent employee, but only the latter period is considered.
In 2010, a system of time-based promotions in the service was established, which enables medical, dental, and pharmacy officers to move up to higher pay grades.
Last-Minute Placement Instructions
A town hall participant highlighted the problems that medical officers encounter with placement.
“Those who transition from a house officer to a medical officer, they will usually be posted to some other state. Say, for example, I’m from Penang, I’m posted to Sarawak.
“We have a three weeks’ notice on which state we are being posted. But after the three weeks, once we are there, we have to sort out all the logistics issues to let us settle down and work. But most of the time, where we are being posted, the final placement, is not decided by KKM.
“Say, I have to report myself in Kuching. They can send me to Sibu, and I have to report to Sibu [within] one day, and that is actually considered my annual leave,” the junior doctor said.
“Without a government policy, this thing will keep going on and we will see more and more people raising this complaint.”
Why Make It Difficult To Become A Specialist?
A town hall participant brought up the issue of financial struggles faced by doctors who undertake subspecialist training and have to rely on their Employees Provident Fund (EPF) retirement savings for allowances and training fees.
“You may ask, ‘Why are you a specialist and not having enough funds?’ At the current moment, let’s say a person were to do their subspecialist training in Australia, for example. What happens is the cost for subspecialty training is not fully covered for.
“Let me give an example. The pelan perancangan of KKM letterhead says tempoh for overseas training is one year, but the allowances provided for are only nine months. What happens to the balance of three months?” he said.
According to the doctor, subspecialist trainees who are single and have no dependents could spend around RM150,370 during their three-year training period, only to receive no compensation upon completion.
“The worst part is that the bonds have been increased from RM25,000 previously to RM600,000 and the bond period has also increased. The amount of increment is 2,000 per cent. If you look at the latest statistics on people who do subspecialty training, the rates have dropped,” the subspecialist said.
A doctor later shared how he continues to be at the UD56 pay grade after over a decade of being in the same position. “I am still UD56,” he said.
“When I came to my hospital, that was 15 years ago, there was a houseman there which I trained – part one, part two, and then MRCP [sic] – she is also now, UD56.
“I’ve seen eight deputy director-generals (DG), four DGs, and I’ve seen five ministers, and I’ve seen four government changes, still UD56.
“How is the minister going to overcome this? [sic] KKM will always [sic] JPA rate. But JPA’s rate is stagnant only,” the doctor said.
Most Doctors Face Abuse From Patients Who Endure Long Waiting Times
Speaking in Bahasa Malaysia, an emergency medical officer asked if there was a “protective mechanism” that could be implemented to support frontline health care workers in both hospitals and klinik kesihatan (public health clinics) facing abuse from patients due to long waiting hours. The officer’s quotes have been translated into English.
“We have SISPAA in place for the public to file complaints against health care staff. But is there a system that acts as a protective mechanism for health care staff where they can file their complaints so that MOH’s top management are aware that their staff are being abused, not by fellow workers, but by the public?
“For instance, at my workplace in the emergency department, we are [sic] and there is currently no special cubicle for the green zone. So that means, in one zone, there will only be one medical officer, in a particular shift, to attend to about 30 to 40 patients at one time.
“So at that time, there may be patients who may have to wait more than six hours, and those who are waiting in the green zone, if they have to be warded, some may even be forced to wait up to 24 hours at the waiting counter in the green zone.
“So when it’s a 24-hour wait, the medical officer then has to see the patient, and at the same time, deal with abuses from the patient. I’m not blaming the patient, but I want to know if there is a protective mechanism for medical officers who serve, especially in the first-line, who are dealing with patients,” the doctor said.
The doctor explained that the hospital currently has a “Code Grey” system to manage the situation.
“The problem is when there’s too many patients, I don’t think officers have time to activate Code Grey etc, especially in the green zone. Some hospitals have designated times. For example, at 2.30pm, we have to complete all cards that come to us. As an MO (medical officer), for example, an evening shift should finish at 10pm, but we often go back at 3am, 4am,” he said.
“I think this is not only happening at my hospital, but other hospitals also have the same problem. So I think, if there is a new mechanism instead of just SISPAA where the patient can file a complaint against us and the hospital management will automatically look for the fault of the medical officer, but there is another system where the medical officer can also express problems that occur in the green zones or at klinik kesihatan.”
The town hall moderator asked the doctors in the room if they had ever experienced abuse from patients before, and “around 70 to 80 per cent” appeared to have raised their hands in response. “Something that is quite prevalent, lah,” commented the moderator.