There is no single measure that is 100 per cent effective in preventing the spread of the SARS-CoV-2 virus which causes Covid-19. Many measures other than vaccination are needed in the battle against Covid-19.
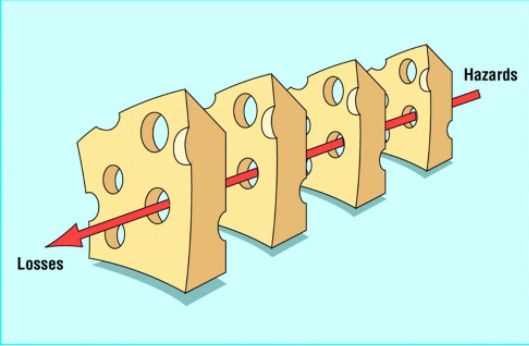
Swiss Cheese Model In Human Error
James Reason put forward the Swiss cheese model to address the problem of human fallibility in the management of error. There are defences, barriers and safeguards in the systems approach.
In an ideal world, each defensive layer would be intact. However, in the real world, the defences are more like slices of Swiss cheese, with holes continually opening, shutting and shifting locations, much like that in the cheese.
Holes in any one slice do not normally cause an adverse outcome. However, when the holes are momentarily in alignment, hazards are brought into damaging contact with victims, which will be patients in health care.
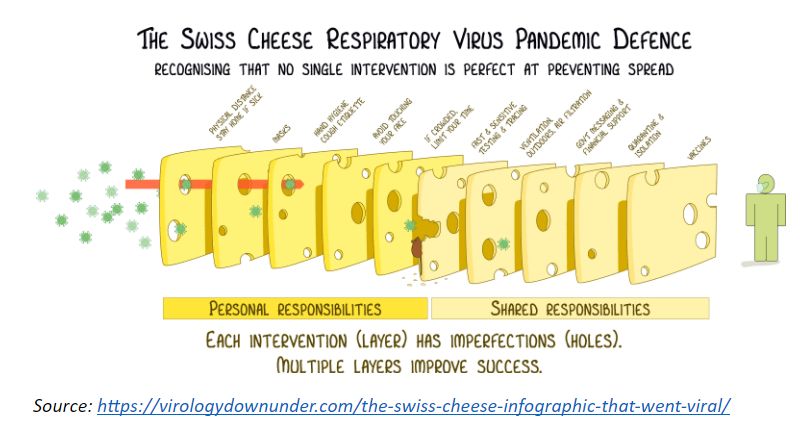
Swiss Cheese Respiratory Virus Pandemic Defence
Ian Mackay, an Australian virologist, adapted Reason’s Swiss cheese model for Covid-19 and created the Swiss cheese Respiratory Virus Pandemic Defence with his colleagues.
Additional slices, each representing one of the defences against the virus, were added to Reason’s model. None of the slices are perfect with each having holes, which represent the measure’s flaws, that allow the virus to find a way through.
Yet with several slices, the likelihood that the virus will be stopped by one of the measures is increased.
There are personal and shared responsibilities in the model. Consider each slice.
Covid-19 Vaccines
Vaccines are generally regarded as one of the most potent measures in the defence against Covid-19.
The first real-world effectiveness of the Covid-19 vaccine was reported by Israel, which launched its vaccination programme on December 20, 2020, nine days after the United States Food and Drug Administration authorised the use of the Pfizer vaccine.
All who were vaccinated by the Clalit Institute for Research, which is the country’s largest health care provider, from December 20, 2020 to February 1, 2021 were matched to unvaccinated controls in a 1:1 ratio according to demographic and clinical characteristics, with each group comprising 596,618 persons.
Two doses of the mRNA vaccine reduced symptomatic cases by 94 per cent, hospitalisation by 87 per cent, and severe Covid-19 by 92 per cent. The effectiveness after one dose, during Days 14 to 20, was 57 per cent for symptomatic cases, 74 per cent for hospitalisation, and 62 per cent for severe disease.
The estimated effectiveness in preventing death was 72 per cent in the two to three weeks after the first dose. However, there was insufficient data to produce an estimate on the reduction in mortality in those who received two doses.
The United States Centre for Disease Control reported that 75 million people had been fully vaccinated from December 14, 2020 to April 13, 2021. There were 5,814 vaccine breakthrough infections i.e. people who had the virus detected on a respiratory specimen collected ≥14 days. The numbers in this cohort (i.e. 0.00775 per cent of total), comprised 2,622 (45 per cent) among people ≥60 years; 3,752 (65 per cent) females; 1,695 (29 per cent) who were asymptomatic; and 396 (7 per cent) who were hospitalised and 74 (1 per cent) who died.
Of the 396 hospitalised, 133 (34 per cent) were asymptomatic or hospitalised for a reason not related to Covid-19, and of the 74 fatal cases, 9 (12 per cent) were reported as asymptomatic or the patient died due to a cause not related to Covid-19.
The Health Ministry announced that 40 Malaysian health care workers who had completed two doses of the vaccine, developed infection, but the infection was less severe.
No information was provided about the clinical characteristics of those affected and the numbers in the cohort.
In short, although vaccination prevented people from getting sick and dying from Covid-19, there is no vaccine yet that is 100 per cent effective, and there is the remote likelihood that one can get infected or spread the virus even after vaccination.
Testing And Contact Tracing
Widespread testing detects people carrying the virus who are unaware they are infected. The polymerase chain reaction (PCR) test is time-consuming and expensive, with specific requirements which not every laboratory might have.
The antigen and the recently introduced saliva tests are rapid tests, but might miss some cases as they are imperfect.
A contact tracing system tracks down those who have been in close contact with a positive case. But the system has to be fast and reach between 80-100 per cent of the contacts for it to be effective in preventing transmission.
The use of digital technology increases its effectiveness, but alas, much of contact tracing in Malaysia is still done manually.
Quarantine And Self-Isolation
Most countries require Covid-19 positive people or who are suspected to be so, to be quarantined either in a health care facility or at home. Some countries also require travellers to quarantine.
The objective is to avoid spreading the infection to others. But there are instances of non-compliance by a few segments of society.
Outdoor Socialising, Ventilation And Air Filtration
Fresh air reduces the likelihood of infection and the ultraviolet radiation from sunlight can destroy any virus left on surfaces. But the risk outdoors is not reduced to zero.
The likelihood of viral spread is greater in crowded and closed spaces, particularly if they are poorly ventilated. The greater the airflow, e.g. by opening the windows, the less likely the spread, but the danger is not completely diminished.
Hand Hygiene, Cough Etiquette And Avoidance Of Face-Touching
Frequent hand washing, cough etiquette and avoidance of face-touching can reduce the likelihood of transmission, but the risk of aerosol spread remains.
It is regrettable that many of the public messages in recent times do not emphasise these simple individual measures.
Masks
Masks and face coverings can block transmission of viral droplets from coughing, sneezing and speaking. But the virus also spreads by aerosols.
As such, even the highest-grade masks are not completely foolproof.
Different masks have different filtration efficiencies, e.g. surgical masks offer more protection than cloth masks. Moreover, masks need to be worn correctly and used constantly by enough members of society to make a difference.
Physical Distancing
Keeping two metres away from another person reduces the likelihood of transmission. But because the virus also spreads by aerosols, one could still get infected, even if you are more than two metres away from a positive person.
Science Based Policies
The US and Brazil, with more than 550,000 and 370,000 deaths respectively, provide examples of the consequences of failures to adhere to science-based policies.
Deborah Birx, the Trump White House coronavirus co-ordinator, said, “The first time we have an excuse. There were about a hundred thousand deaths that came from that original surge. All of the rest of them, in my mind, could have been mitigated or decreased substantially.”
Despite surging infections, with more than 66,000 deaths alone in March 2021 and the health care system near collapse, Brazilian President Bolsonaro continues to downplay the threat of Covid-19.
Even when policies are science-based, compliance is critical. The disregard of the government’s standard operating procedures (SOPs), particularly by some public figures, and disparity in enforcement of the SOPs send very negative messages to the citizenry.
Summary
It is evident that no slice of the Swiss cheese model provides 100 per cent protection against viral transmission. The cheese’s holes will constantly open, shut and shift location, depending on individual behaviours.
Even when there is widespread vaccine coverage, multiple measures are needed to stop the holes from aligning and letting the virus through.
It is only by using a number of slices, i.e. anti Covid-19 measures, that there is the best likelihood of protection.
Policies have to be based on scientific evidence with transparent data analysis that can withstand scrutiny. It is futile to base decisions on wishful thinking.
Last but not least, it is vital to remember that the virus does not discriminate.

Dr Milton Lum is a past President of the Federation of Private Medical Associations, Malaysia and the Malaysian Medical Association. This article is not intended to replace, dictate or define evaluation by a qualified doctor. The views expressed do not represent that of any organisation the writer is associated with.








