By David Heymann, London School of Hygiene and Tropical Medicine
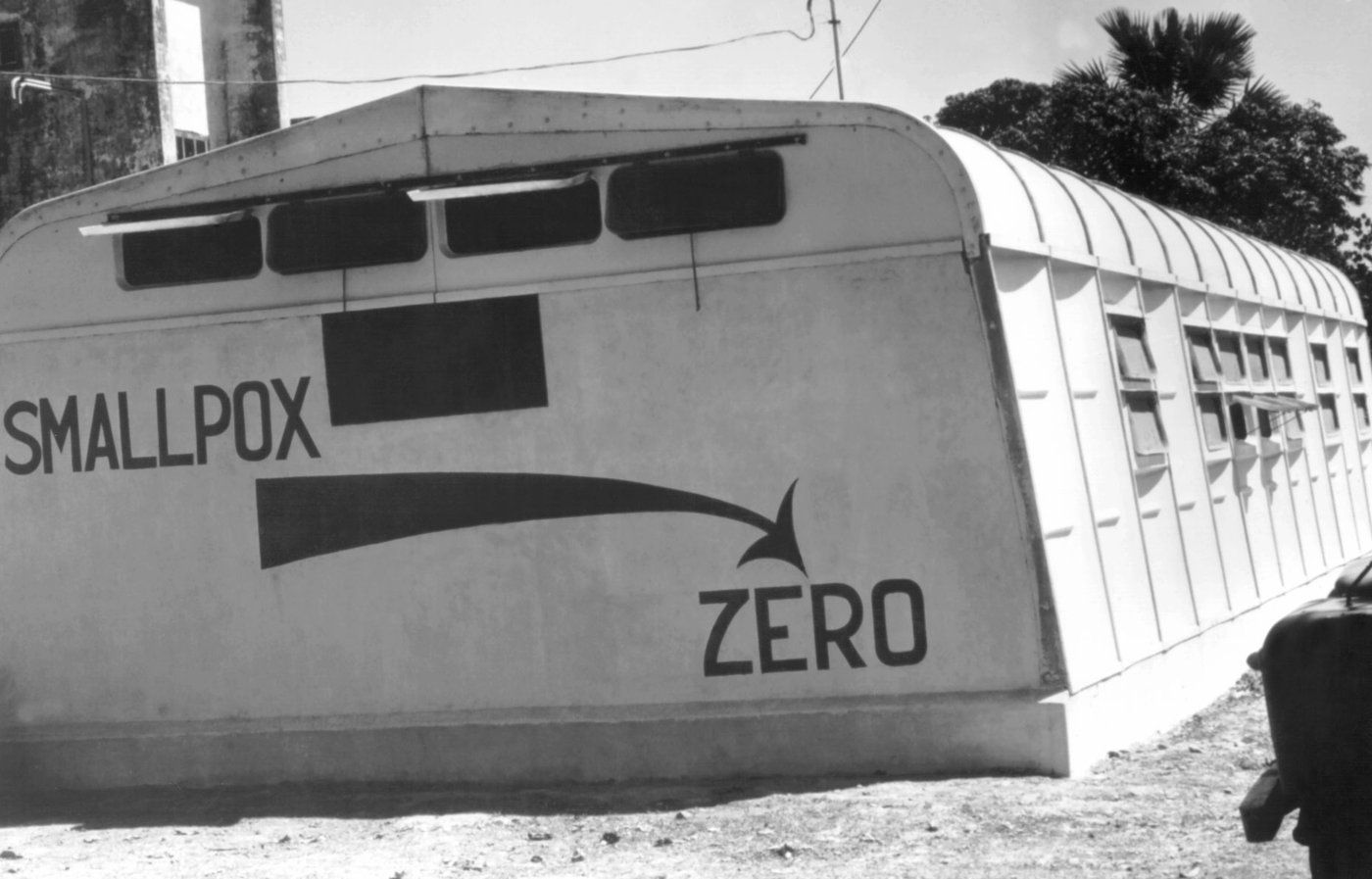
LONDON, Feb 28 – It’s been over 40 years since smallpox was declared eradicated by the World Health Organization (WHO) — the only human disease to reach that milestone so far.
The declaration brought to an end a disease that had plagued humanity for at least 3,000 years and was estimated to have led to the deaths of 300 million people in the 20th century alone.
Yet equitable vaccine distribution challenges during the recent Covid-19 pandemic raise the question as to whether a similar smallpox eradication effort would be possible today.
Smallpox had a massive impact around the world.
In 1967 — the year smallpox eradication efforts were intensified — there were an estimated 2.7 million deaths from the disease.
Compare this to estimated deaths from other infectious diseases in 2019, and smallpox would still dominate, even without calculating the greater theoretical number of smallpox deaths that would have been proportional in 2019 due to population increases.
In contrast, diarrhoeal diseases accounted for an estimated 1.5 million deaths in 2019.
The completion of smallpox eradication in 1980 likely happened just in time.
AIDS was first identified the following year, and HIV, the virus that causes it, spread rapidly throughout the world.
In 1985, a military recruit in the United States had a serious reaction to a smallpox vaccination, which led to his death six months later. US military personnel have been routinely vaccinated against smallpox – despite its eradication – because of the fear it might be used as a biological weapon.
At the time he was vaccinated, the recruit was infected with HIV, which caused decreased immunity and led to the vaccine reaction and the recruit’s death. Only later did it become known that the smallpox vaccine poses safety concerns for HIV-infected people.
If smallpox hadn’t already been eradicated before HIV started spreading rapidly, we would have lost the window of opportunity to do so.
Smallpox eradication was possible because the smallpox virus has no reservoir in nature outside humans — like polio and measles, but unfortunately not the case with other diseases such as COVID and mpox.
There was an effective vaccine, it was possible to identify each person infected due to the distinctive rash, so no infections were missed — again more of an issue with Covid and asymptomatic infections — and nations were more willing to work together.
Public health workers from around the world — including from the US and USSR — worked side by side coordinating strategy, logistics and vaccine donations to accomplish eradication despite the political tensions of the Cold War.
Health was, and in many instances today remains, a neutral point for collective public health action, such as in the eradication of polio and guinea worm.
The strategy to eradicate smallpox was simple: identify those who had signs and symptoms of smallpox, with health workers searching in markets, at religious gatherings and from door to door.
Ensure that those with smallpox had healthcare support and were isolated to prevent spread to others, vaccinate their contacts and neighbours, and in some instances send specimens to remote laboratories for confirmation.
Searching for smallpox was costly and time-consuming for health workers. Sending specimens for confirmation was likewise costly, and results were slow. Vaccinators often required hand-drawn maps to find those who were infected.
But the efforts of some 10,000 health workers who administered an estimated half a billion vaccinations led to the final achievement of the disease’s eradication.
While the intensified effort is estimated to have cost global donors US$300 million, on top of country contributions, it’s now thought to have saved the world more than US$1 billion a year since 1980.
Technical innovations available today would have helped facilitate the eradication of smallpox, as they are now doing for the eradication of polio and guinea worm.
Smartphones, for example, allow community members to participate in their own monitoring by reporting suspect infections through dedicated applications.
More sophisticated point-of-care diagnostic tests can confirm diagnosis in hours rather than weeks.
Environmental surveillance at multiple sites through the use of genetic sequencing allows for the presence of diseases to be detected, even when human infections have not yet been found.
Geopositioning and digital cartography have brought mapping into the 21st century.
Surveillance for infectious disease eradication has been turned upside down since the days of smallpox eradication, with communities reporting to health workers rather than health workers travelling to communities to identify those with infections.
In 2011, a second infectious disease was declared eradicated by using an effective vaccine and technologies such as participatory surveillance and geopositioning.
That disease was rinderpest, a highly fatal disease of domesticated cattle that at times spread to other domesticated animals and wildlife.
With continued use of new technologies developed since the days of smallpox eradication, polio and guinea worm may also soon be relegated to the history books.
Smallpox eradication was the first time the world came together to ensure equitable distribution of a vaccine, and polio eradication continues along the same path.
The recent example of the Covid-19 pandemic, when a special international mechanism called COVAX was established to ensure more equitable access to vaccines, demonstrates the importance the international community continues to place on equitable distribution of vaccines as has been accomplished for smallpox and polio.
Becoming complacent, or letting geopolitics and national rivalries impede international collective action could prevent successes such as those of smallpox and other disease eradication programmes.
David Heymann is Professor of Infectious Disease Epidemiology at London School of Hygiene and Tropical Medicine.
Article courtesy of 360info.