PETALING JAYA, Nov 15 – Only 26 per cent of people believe that pneumococcal vaccination is necessary for adults with medical conditions, according to Dr Pang Yong Kek, co-chairman of the Prevent Pneumococcal Pneumonia Initiative and associate professor at the University of Malaya.
Dr Pang highlighted the low awareness of pneumococcal vaccine among the general public, revealing that only 24 per cent of adults recognise the importance of vaccinating the elderly against pneumococcal pneumonia.
“This is alarming. The awareness among the public is generally still quite low. What needs to be done? Of course, I think actually not just health care providers, I think the media play a very crucial role as well to step up efforts to increase awareness of the public that we need to address this very deadly disease.
“In general, I think that we can say that individuals who are very young, very old, those with chronic conditions and are immunocompromised, should be vaccinated because they are highly vulnerable.
“Part of the reason is because when we are very young, below five years old, our immune system is still not mature. And after that as we get older, our immune system becomes more mature and then we have natural immunity that even if we get an infection, it is less likely for us to actually die of any infection.
“But as we get older, our immune system again gets older. This is actually a process called immune senescence. Our immune system becomes older and less effective, and that is the reason why we should get ourselves immunised to boost our immunity for certain infectious agents,” said Dr Pang at the Prevent Pneumococcal Pneumonia Initiative launch event held at the Petaling Jaya Sheraton Hotel last November 8.
Due to immune senescence, the risk of contracting pneumococcal disease significantly increases after the age of 40, Dr Pang added.
Data from the Surveillance Atlas of Infectious Diseases in 2021 shows a rise in the risk of contracting pneumococcal pneumonia from 10.7 per cent for people aged 25 to 44 to 27.6 per cent for people aged 45 to 64, and further to 49.4 per cent for individuals aged 65 and above.
“For those who are more than 65 years old, they are four times more likely to be infected with pneumococcal pneumonia compared to the general population. And if they do get pneumococcal pneumonia, there is a five time risk for them to require hospitalisation.
“More alarmingly, if they have pneumococcal disease, you can see the mortality is concentrated in those who are older. Pneumonia can occur at any age, but in the elderly population there is a 60 per cent of chance of them dying if they get pneumonia, and if they get bacteremia, that is even worse because 80 per cent of elderly patients compared to the general population die because of the infection.”
Pneumonia is an infection of the lungs where the alveoli become inflamed and fill up with fluid. This often results in an impairment of gas exchange. It causes cough with phlegm or pus, fever, chills, and difficulty in breathing. A variety of bacteria, viruses, and fungi can cause pneumonia.
In 2022, the Department of Statistics reported that pneumonia was the leading cause of death in Malaysia, accounting for 13.3 per cent of all deaths. For women, it was the second leading cause of death with 11.5 per cent of women dying from the disease. For men, it was the third leading cause of death with 10.8 per cent of men dying.
Pneumococcal disease is a name for any infection caused by the bacteria called streptococcus pneumoniae, or pneumococcus. These infections can range from ear and sinus infections to pneumonia and bloodstream infections.
The bacteremia Dr Pang referred to is when there is bacteria present in the bloodstream.
The National Immunisation Programme (NIP) in Malaysia vaccinates babies against pneumococcal diseases before they are eight months old. The first dose is given when the child is four months old, and the second dose is given when the child is six months old. A booster shot can be given when the child is 15 months old.
However, the United States’ Centers for Disease Control and Prevention (CDC) recommends that certain high-risk groups take a second dose of the vaccine.
Dr Pang said people who are considered to be at-risk are those who have chronic conditions such as diabetes mellitus, chronic heart disease, and chronic obstructive pulmonary disease (COPD).
This means that a large sub-section of the Malaysian population is considered at-risk. The National Health and Morbidity Survey (NHMS) 2019 states that one in five adult Malaysians are living with diabetes, one-third are living with hypertension, and half are overweight or obese.
A joint report last year by the Ministry of Health (MOH) and the World Health Organization (WHO) further revealed that annual direct health care costs from diabetes in Malaysia total about RM4.4 billion, 227 per cent higher than cancer (RM1.3 billion) and 11 per cent higher than cardiovascular disease (RM3.9 billion).
“If we have other medical conditions like diabetes, our risk will increase like three times of getting pneumonia. And if you have heart disease, which a lot of people may not associate with lung infection, the risk is four times higher. And if you have a lung condition called COPD, the risk will increase about nine times. So, it’s not only actually the individual medical condition, if you have a more medical condition, this risk will stack up.”
Citing a 2015 study titled “Redefining risk categories for pneumococcal disease in adults: critical analysis of the evidence” published by the International Journal of Infectious Diseases, Dr Pang demonstrated how people with stacking chronic conditions have higher chances of contracting pneumococcal diseases.
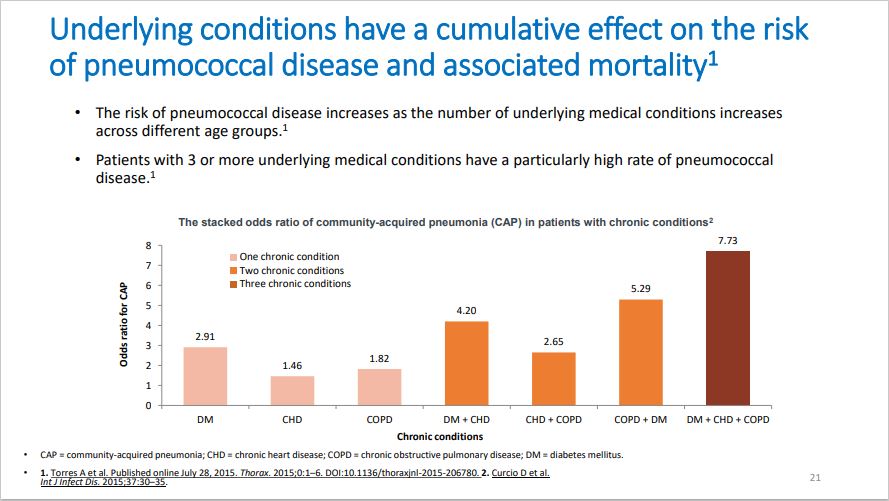
The study shows that people who have a single chronic condition have low chances of contracting community acquired pneumonia (CAP).
For example, people who only have DM have a 2.91 ratio of contracting CAP, but people who have two chronic conditions such as DM and CHD have a 4.20 ratio of contracting CAP. Finally, people who have three chronic conditions such as DM, CHD and COPD have a 7.73 ratio of contracting pneumococcal disease.
In addition to chronic conditions, an American study titled “Rates and costs of invasive pneumococcal disease and pneumonia in persons with underlying medical conditions” published in the BMC Health Services Research Journal revealed that people living with HIV and other immunocompromising conditions are also at increased risk for pneumococcal disease.
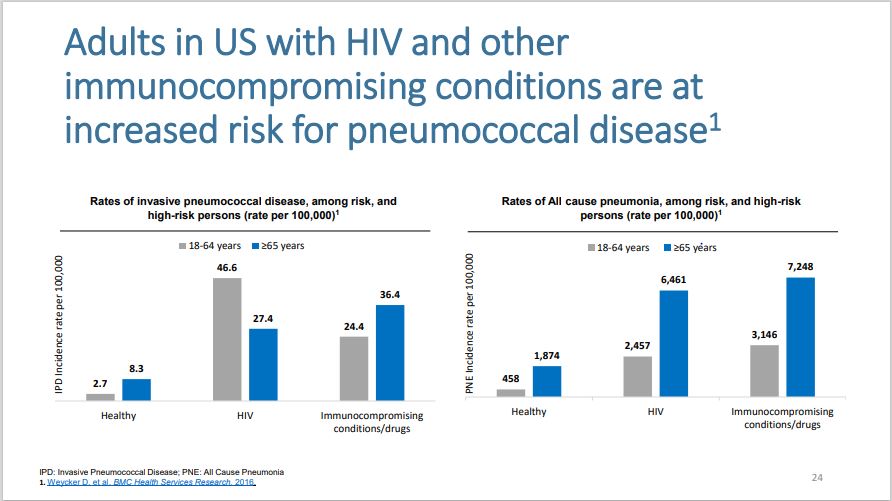
HIV patients between the ages of 18 to 64 years have an incidence rate of 46.6 per 100,000 people contracting the disease, and people in the same age group living with immunocompromising conditions have a 24.4 incidence rate.
Patients aged 65 years and above who have HIV have a 27.4 incidence rate, while those with immunocompromising conditions have a 36.4 incidence rate.
There are two types of pneumococcal vaccines available: PCV13 and PPSV23. Dr Pang held that recommendations call for the mixing of the two vaccines for at-risk individuals and the elderly.
The main difference between the two vaccines is that the PCV13 vaccine is a protein conjugate vaccine while the PPSV23 is a polysaccharide vaccine. The main advantage of the PCV13 vaccine, according to Dr Pang, is that protein conjugate base vaccines stimulate long-term memory of new cells.
The polysaccharide base vaccine, on the other hand, tends to offer people good protection for the first one or two years. After that, the immunity wanes.
“Immunity will actually become weaker over time because the polysaccharide vaccine generally stimulates the P cell. The P cell is responsible for producing antibodies. It does not actually translate into long term memory, which is located in the plasma cell.
“Whereas the conjugate protein, the advantage is actually also stimulating the plasma cell, and this memory will be retained for a much longer time.
“How long, we do not know, but based on whatever evidence we have, it is at least four to five years. But because no study actually was done beyond four to five years, we don’t know what the long-term efficacy is like.”
The PCV13 targets 13 valents of the pneumococcal serotype. This means that adults who are inoculated with this vaccine are protected against serious infections caused by 13 out of the 90 types of pneumococcal bacteria.
The PPSV23, on the other hand, protects people against 23 types of pneumococcal bacteria.
Apart from the vaccine, people can take other preventive measures such as regularly exercising, maintaining good hygiene, eating healthy, and quitting smoking.








