The immunisation of pregnant women for the protection of both the mother and the baby is not something new. In 1879, maternal immunisation with vaccinia conferred protection against smallpox for infants.
Maternal immunisation with the whole cell pertussis (wP) vaccine in 1938 protected babies against whooping cough.
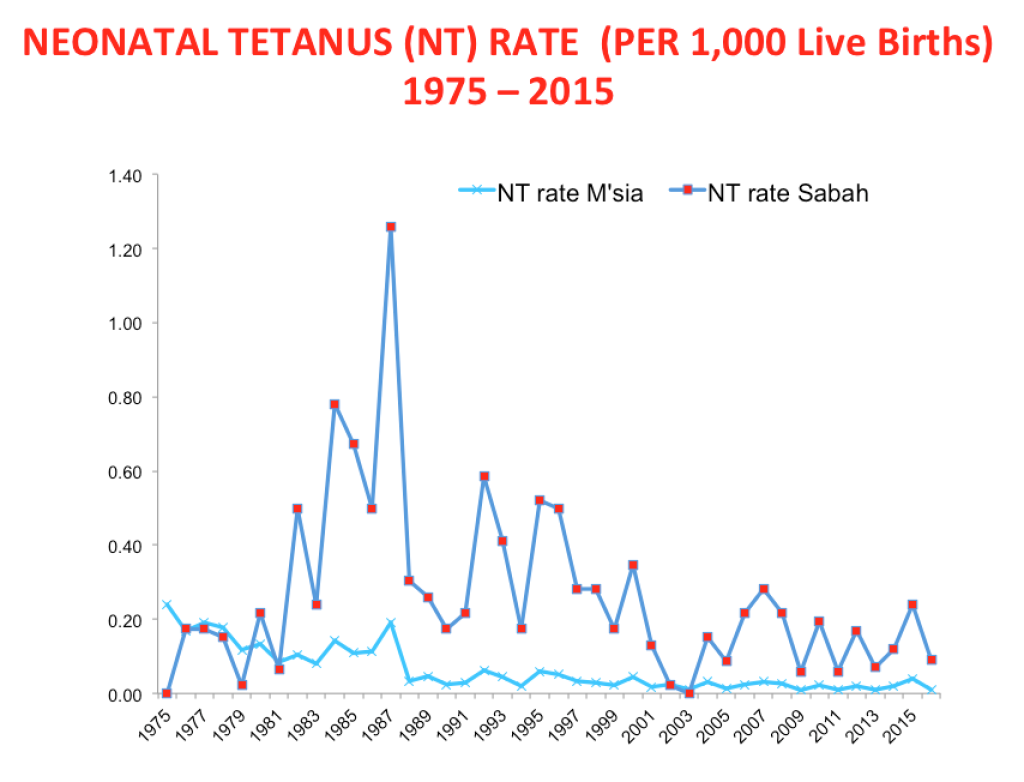
Tetanus toxoid (TT) given to pregnant women prevented maternal and infant deaths in New Guinea in 1961. Malaysia introduced TT for gravid women in 1976.
This has been associated with a dramatic decline in the number and incidences of neonatal tetanus. There were 108 cases of neonatal tetanus in 1976 versus 31 cases in 2018 (all recorded within Sabah’s illegal immigrant population, with six deaths).
However, elimination of neonatal tetanus can only be achieved if the maternal TT programme and the hexavalent (TDap-IPV-Hib-Hep B) Expanded Programme on Immunisation is better accessed by the immigrants, refugees, indigenous peoples, and pockets of rural and urban poor.
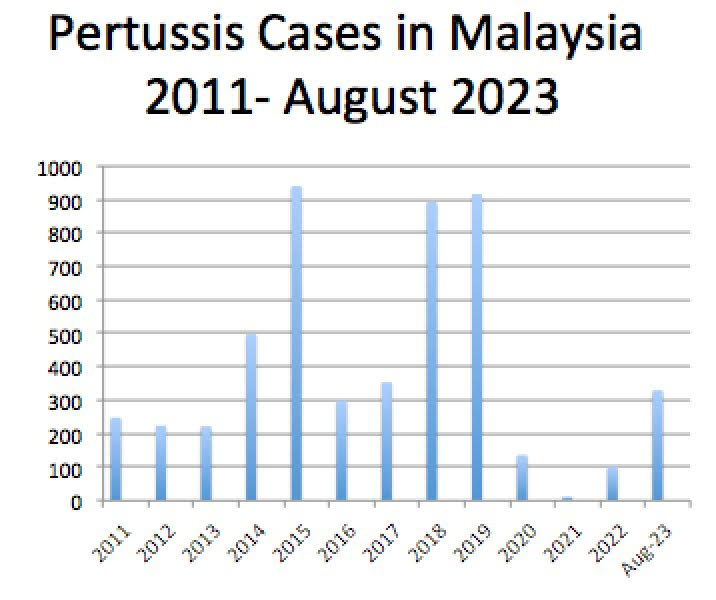
The graph below shows pertussis cases in Malaysia from 2011 to August 2023. The true incidences of pertussis are likely to be higher than reported, due to under-diagnosis and under-reporting.
More granular data showed that in 2020, 98/136 (72 per cent) cases were below six months of age. A careful analysis of the cases from 2019 and 2020 revealed that 25/56 (45 per cent) cases were younger than two months old. Up until August 2023, 189/329 (57 per cent) cases were below 12 years old.
Many of the confirmed cases of pertussis were either too young for the pertussis vaccine (unvaccinated) or did not receive sufficient doses of the vaccine for their age (under-vaccinated).
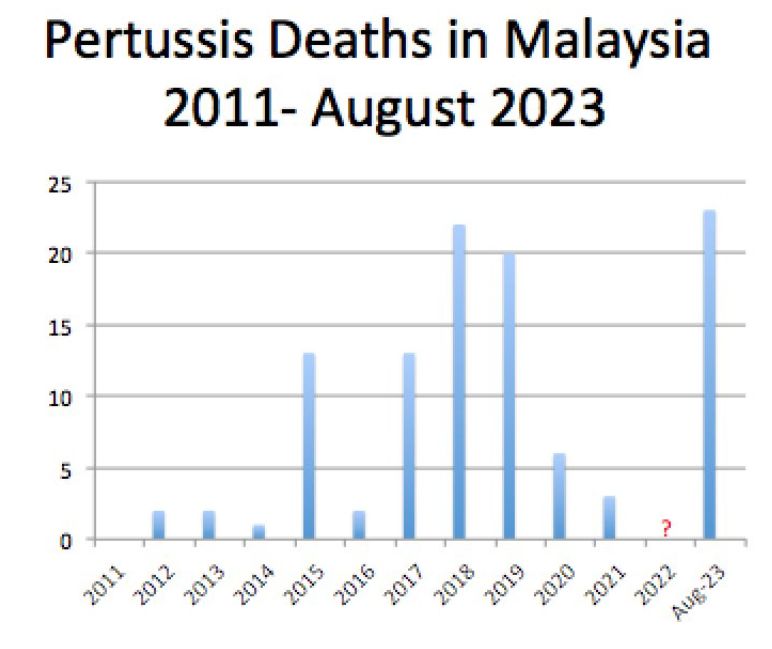
Even more tragic is the fact that up until August 2023, there have been 24 pertussis deaths, and 19 (79 per cent) of these children were younger than five months. This is the highest pertussis mortality rate since 2011, exceeding pertussis mortality in 2018, where 19 (86 per cent) out of the 22 deaths were younger than 6 months old (see graph below).
Pertussis illness requiring admission to the paediatric ICU is referred to as critical pertussis. In a local study, infants aged less than or equal to three months old were at high risk of developing critical pertussis.
This is similar to other studies which report that about 75 per cent of pertussis-related deaths occur in infants less than three months of age. (5,6,7).
They also showed that 93 per cent of infants less than three months of age with pertussis required admission to hospitals.
A hospital-based study conducted in four countries demonstrated that household members were responsible for 76 to 83 per cent of the transmission of laboratory confirmed pertussis to infants less than six months. Older individuals represent potential sources of infection, potentially transmitting pertussis to unvaccinated or partially vaccinated infants.
In a local study, almost two-thirds of the patients had acquired pertussis from their family members.
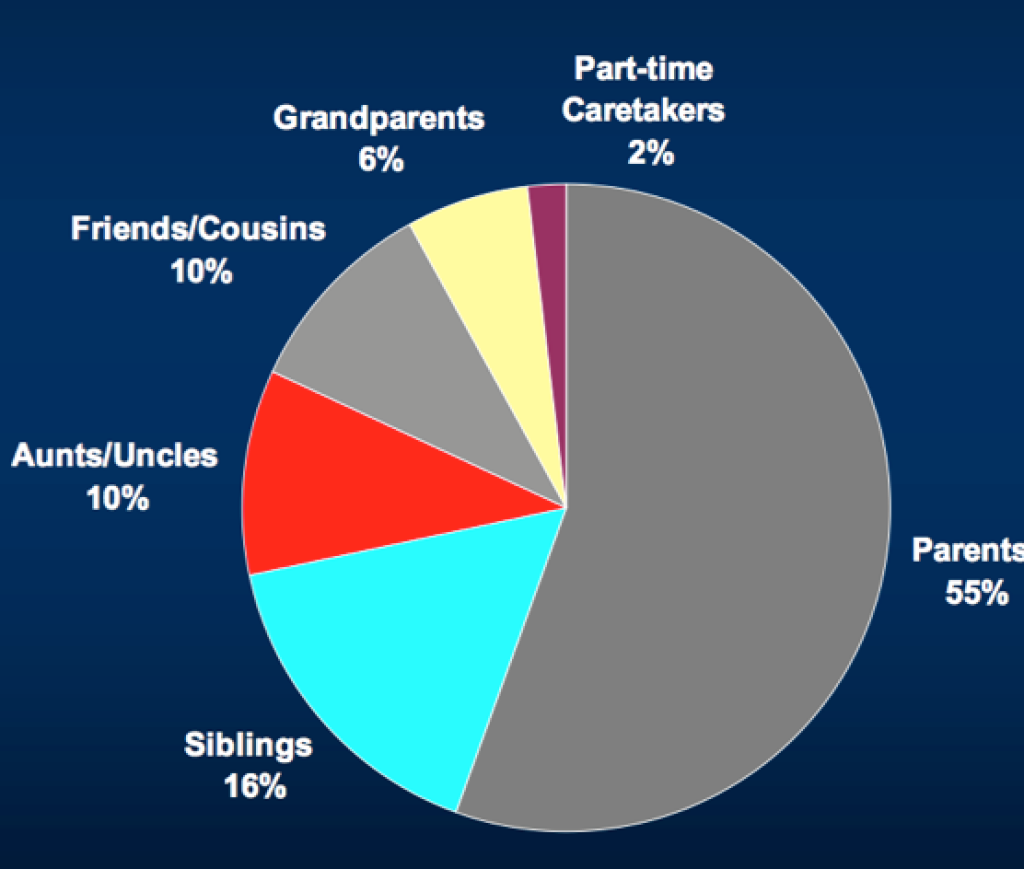
Undoubtedly, additional vaccination strategies are required to protect these vulnerable infants from pertussis. These include booster vaccinations for schoolchildren, adolescents, and adults.
A cocooning strategy among immediate family members can prevent the transmission of pertussis to vulnerable infants.
In October 2011, the United States’ Advisory Committee on Immunization Practices (ACIP) recommended that unvaccinated pregnant women receive a dose of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in an effort to reduce the burden of infant pertussis. In the following year, the ACIP voted to recommend the use of Tdap for every pregnant woman.
Following Tdap vaccination, the pregnant mother will make protective antibodies and can pass high levels of them to her baby before birth, providing the newborn with protection against pertussis in early life.
Similarly, the mother will be protected from pertussis around the time of delivery, making her less likely to become infected and transmit pertussis to her infant.
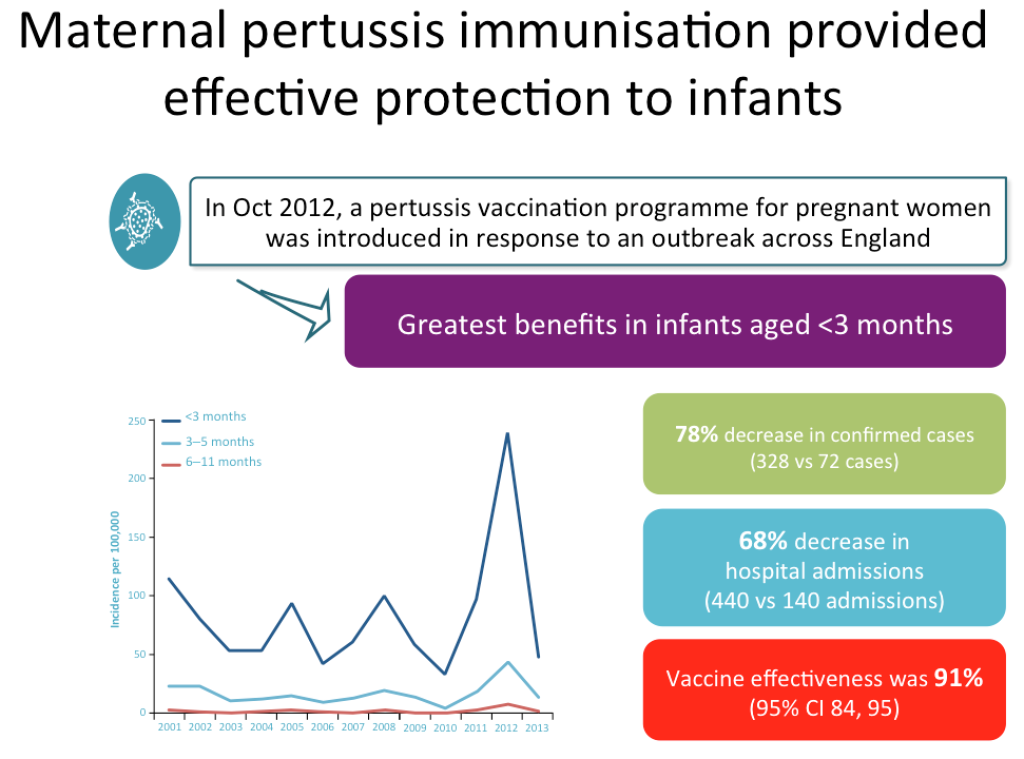
In October 2012, a pertussis vaccination programme for pregnant women was introduced in response to an outbreak across the United Kingdom. The study demonstrated a 78 per cent decrease in confirmed pertussis cases and a 68 per cent decrease in hospital admissions, with a vaccine effectiveness of 91 per cent.
The greatest benefits were enjoyed by infants aged less than three months old. (see graph below)
A surveillance study from July 2014 to November 2015, taking place three years following the introduction of the Tdap vaccination, showed sustained effectiveness of the maternal immunisation programme in the UK. The vaccine effectiveness (VE) against pertussis was 88 per cent, with a 95 per cent success rate against pertussis-related deaths.
Maternal Tdap immunisation has since been demonstrated to achieve a significant decrease in pertussis mortality and morbidity in Spain, Argentina, Colombia, and other countries.
Several prospective and observational studies including a study by the UK’s Medicines and Healthcare Products Regulatory Agency (MHRA) of 20,000 vaccinated pregnant women found no evidence of risks to pregnancy or babies.
A number of countries, including the UK, the US, Argentina, Belgium, Spain, Australia, and New Zealand, currently recommend Tdap vaccination for pregnant women.
In 2024, the Tdap vaccine will be included in Malaysia’s National Immunisation Programme to protect mothers and babies against pertussis. For now, pregnant women can get their Tdap and influenza vaccines from general practitioners (GPs) and obstetricians.
Maternal immunisation represents a new frontier in vaccinology and can protect infants from vaccine preventable diseases (VPD), thus improving infant outcomes.
More recently, the respiratory syncytial virus (RSV) vaccine was approved by the US Food and Drug Authority and the European Medicines Agency (EMA) for maternal immunisation to protect babies from the scourge of RSV acute bronchiolitis.
Meanwhile, research is ongoing to find maternal vaccines to prevent the threat of Group B streptococcus, cytomegalovirus, Zika virus, and others.
Dr Musa Mohd Nordin and Dr Husna Musa are paediatricians.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.






