The Ministry of Health (MOH) recently announced the roll-out of the catch-up pneumococcal vaccination programme (CHUPP) on World Immunization Day, May 31, 2023.
It will be made available for all four and five-year-olds (2018 and 2019 birth cohorts) for a one-year period until May 31, 2024.
This will supplement the 2+1 pneumococcal vaccination programme which commenced in December 2020. The uptake of this programme was reported to be 95 per cent and 93 per cent for the first and second dose of the Pneumococcal Conjugate Vaccine 10 Valent (PCV10) respectively, from January to September 2021.
I suspect the uptake of the PCV10 has substantially declined during the Covid-19 pandemic, caused by various factors, including lockdowns, social distancing, vaccine hesitancy, and refusals.
The CHUPP programme will administer the PCV13, which has a wider coverage of the pneumococcal serotypes in Malaysia. A study by the Institute of Medical Research (IMR) of Invasive Pneumococcal Diseases (IPD) in children below 5 years old for the period 2014 to 2017 showed that the PCV13 had 88.2 per cent coverage, whilst the PCV10 had 64.1 per cent coverage.
The CHUPP programme will protect a larger cohort of vulnerable children below 5 years of age, as well as providing better coverage of the responsible pneumococcal serotypes in Malaysia.
This will contribute considerably towards the attainment of herd immunity, with the elimination of vaccine pneumococcal serotypes in the naso-pharynx and the wider uptake among children below 5 years old.
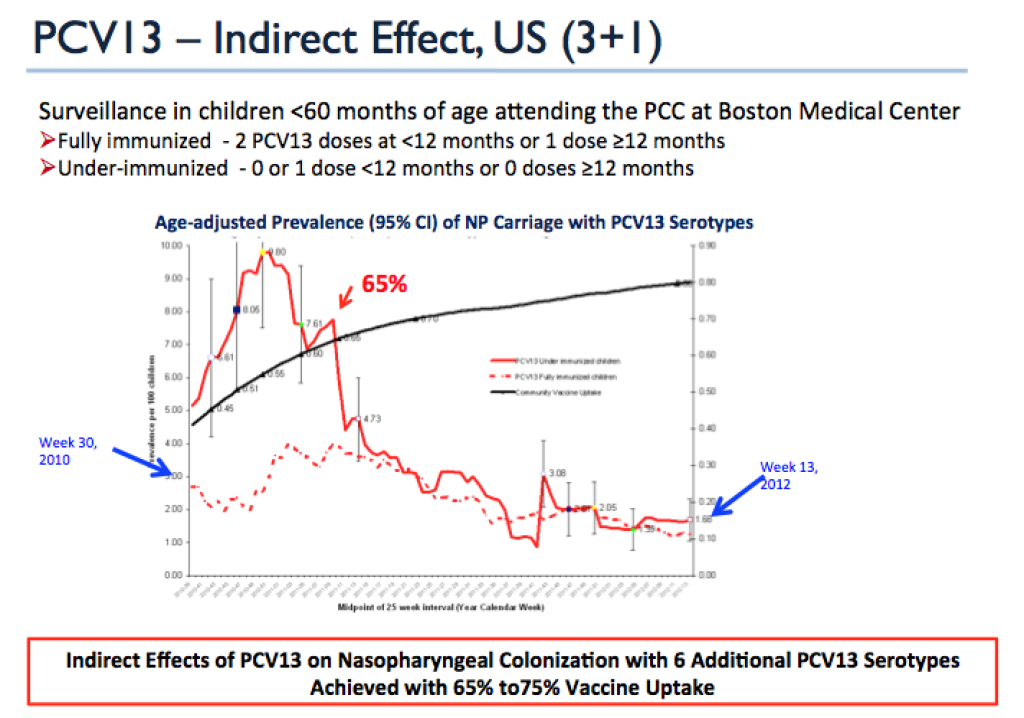
Studies from the United States, France, Israel, and Italy have demonstrated a significant reduction in naso-pharyngeal colonisation after the inclusion of PCV13 in the National Immunisation Programme in children between 3 and 59 months old.
This has been shown to correlate with significant herd effects in those who were unvaccinated. A 30 per cent population-level decline in pneumococcal-related mortality among the non-vaccinated was observed post-PCV13 introduction (2011 to 2013) compared to the pre-PCV period (2000 to 2007) in Denmark.
Malaysia’s 2+1 and CHUPP schedule needs to achieve at least a 65 to 75 per cent vaccine uptake to achieve this herd effect as forecasted by Pelton, et al in 2012.
The most important rationale for the introduction of the PCV is to prevent deaths, hospitalisations, and serious sequelae from IPD. We do not have impact studies of PCV on IPD in Malaysia, because our programme only started in December 2020, when the Covid-19 pandemic was in full swing, with all of its ramifications on the Expanded Programme of Immunisation (EPI).
Impact studies in countries with PCV13 in their immunisation programmes have shown a more than 90 per cent vaccine effectiveness (VE) for vaccine serotype IPD. Meningitis hospitalisation rates have decreased to 50 to 65 per cent. In the US, IPD admissions have declined by 36 per cent.
In the Gambia, PCV9 was the first vaccine in 20 years to show a significant reduction in all-cause child mortality in a major randomized controlled trial. Seven deaths were prevented for every 1,000 children vaccinated with PCV9 in the Gambia study.
Nicaragua, a beneficiary of the GAVI (Vaccine Alliance) financial assistance, recorded a 34 per cent decrease in all infant mortalities.
Prior to the introduction of the PCV, pneumococcal pneumonia had caused 741,000 deaths among children below 5 years, more than pneumonia deaths from Respiratory Syncytial Virus (130,000), influenza (25,000), and Haemophilus influenza B (290,000) combined. (11,12,13)
PCV caused a 30 to 80 per cent decline for all caused pneumonia. Uruguay’s 2+1 schedule led to a 75 per cent and 90 per cent decrease of pneumonia and empyema respectively.
The impact of PCV on acute otitis media (AOM) is important because it may lead to hearing deficits, which may contribute to delayed speech and learning disorders. The occurrence of AOM is very frequent, and prevention would tip the scales towards favourable cost effectiveness (CE) of the PCV programme.
Pneumococcal AOM has decreased by 75 per cent and all caused AOM by 60 per cent. Ambulatory visits for AOM have declined by 33 per cent, and serious complications from AOM, like mastoiditis and the need for grommets insertion has decreased. Outpatient antibiotics scripts for AOM and non-AOM acute respiratory infections (ARI) has reduced by 43 per cent.
The inclusion of PCV13 in the US’s immunisation programme in 2010 has been associated with a substantial reduction of the incidence of antibiotic resistance for macrolides, cephalosporins, tetracyclines, and penicillin.

The introduction of the PCV in the National Immunisation Programme has had a significant impact on the incidence of IPD, pneumonias, AOM, carriage clearance, herd effects, and antibiotic resistance.
A surveillance of IPDs and its ramifications in Malaysia is pertinent to demonstrate these benefits in the national context. This can only be borne out if all health care professionals, notably family medicine specialists, medical officers, nurses, and allied health care professionals at health centres and district hospitals, general practitioners, and paediatricians get their act together to ensure the 2+1 schedule and CHUPP outreach at least 700,000 of the one million children within the 2018-2019 birth cohort.
A high compliance rate of at least 70 per cent is critical, in order for us to satisfy the 3Cs of a successful vaccination programme, namely Coverage, Coverage, and Coverage.
Dr Musa Mohd Nordin and Dr Husna Musa are paediatricians.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.




