I am Boon Lui, a breast cancer survivor and patient advocate. In 2017, I opted for early retirement from work and formed the Society for Cancer Advocacy and Awareness Kuching (SCAN in short) with a group of like-minded survivor friends.
We spread cancer awareness to the public, highlight important cancer care issues to the concerned authorities, and engage with many fellow patients through our peer support and counselling.
I was first diagnosed with stage 3 breast cancer in 2006. Apart from the left breast removal surgery done in a private hospital in Singapore, I underwent all other treatments at Sarawak General Hospital (SGH) in Kuching, Sarawak, where I have lived since 2000.
All my treatment costs were very affordable with heavily subsidised treatments (including 20 sessions of radiotherapy, eight cycles of chemotherapy and five years of oral hormonal medication for my hormone-positive nature). I had my insurance cover some of the expenses for my surgery in Singapore, after which, my insurance policy ended.
When my breast cancer recurred in 2017, spreading to my right lung, liver and bones, i.e. what we called Metastatic Breast Cancer (MBC), I was recommended by my oncologist at SGH for a new targeted therapy drug to be taken orally. This drug was not, and is still not, funded by our government.
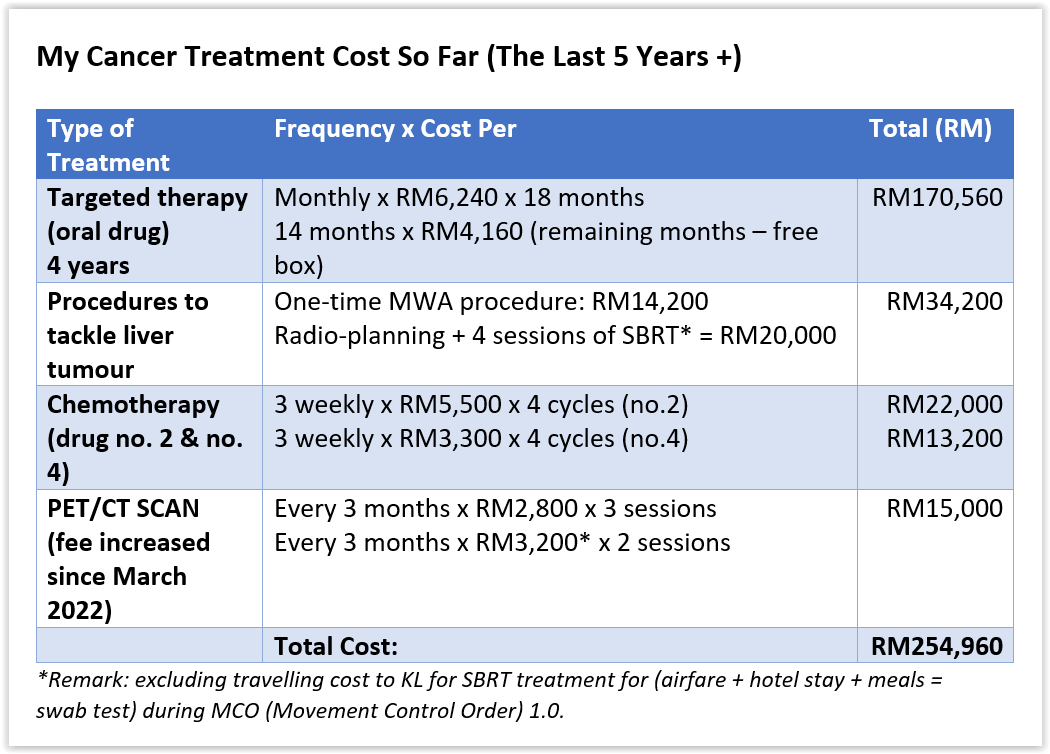
I had to pay out-of-pocket for a good four years in generally stable condition. An exception was in October 2019, when a single-growth tumour in my liver became a terrifying threat.
Advised by my oncologist, I underwent two medical attempts — a Microwave Ablation (MWA) Procedure and an advanced radiotherapy, i.e. SBRT, to tackle this tumour. Both these treatments were only available at private hospitals and were self-sponsored.
The targeted therapy cost more than RM6,000 every month until a patient-assisted programme was made available one-and-a-half years later. I then purchased the drugs at a discounted rate and was given some free boxes later. This drug worked well for me until it lost its efficacy in August 2021, when my PET/CT scan showed new cancer progression.
Since then, my oncologist switched me to an oral chemo drug (funded by the government, September 2021 to January 2022). However, it gave me a mixed response (some cancer spots are stable while some are growing) as shown in PET/CT scan after six cycles.
Soon after, I was given IV (intravenous, i.e. injected via the vein) chemo drugs – no. 1 and then no. 2, which had to be self-purchased because it was not funded by the government. The reason for switching chemo drugs was due to mixed response seen on repeated PET/CT SCAN after 4 cycles each.
I’m now on my fifth line of treatment using a combination of two chemo drugs (funded by the government), as chemo drug no. 2 didn’t work well for me too.
Throughout the last five years with MBC, more than RM254,000 have been paid out from my savings for my treatments, including PET/CT scans (done in the only private hospital in Kuching, Sarawak, with this machine). I’ve been paying RM50,000 annually (or more than RM4,200 every month), excluding living expenses.
My savings are fast depleting.
Though I’m a recipient of the SOCSO invalidity pension scheme starting at the end of 2017, the monthly scheme of about RM1,000 is only meant for domestic living expenses rather than medical treatment.
Nevertheless, I am fortunate to have a financial backup from my past 25 years of earnings. It is a blessing that my treatment has kept me alive thus far.
Now, the question is, what about other metastatic breast cancer patients from low-income and non-income groups such as retirees and single mothers?
The reality is, most cancer patients seeking treatments at SGH are from the B40 group, and a lower percentage is from the M40 group. Even those from the M40 group will have a hard time facing the high drug costs, which are in addition to daily expenses for their families.
Without the financial means, these cancer patients could only be given treatments (be it chemotherapy or radiotherapy, if deemed suitable to help) funded by the government. They will not have access to advanced drugs like the targeted therapy which have to be self-funded and lose out on optimal cancer health care, including increased mortality risk.
Furthermore, patients farther away from Kuching also need to spend substantially on their travelling costs to Kuching, and vice versa.
Affordable cancer treatment is just not there for most Malaysians when their diseases are in advanced stages requiring advanced drugs for their treatments. Can we really claim that our public health care does provide universal health care coverage?
The Ministry of Health may reason that with a limited budget, government funding could only be prioritised for those requiring cost-effective treatment. Rightfully, those in the early stage of cancers with standard or established drugs with a high survival rate have been statistically proven.
Access to health care is a basic human right.
No matter your age, gender, race, ethnicity, where you reside, how much money you make, or any other factor, you have the fundamental right to health care.
The family and community would maintain hope for an extended life of their loved ones with a respectable quality of life if an advanced cancer patient had access to critical care and therapy.
Instead of seeing cancer treatments as a cost or an economic burden, we should start thinking of them as investments.
I earnestly plead with the government to find solutions to get newer drugs to the patients through innovative solutions. Some of which could be:
- Through national health insurance schemes like what countries like Taiwan and Singapore have implemented.
- Giving waivers to cancer patients who contribute to annual tax payments in the past.
- A cancer drug fund could be established. Give incentives to those in the T20 group to contribute to this fund by giving them some form of tax exemption.
The gaps in cancer care in Malaysia are glaring and need to be addressed.
It is projected that there’ll be 66,000 cancer cases annually by 2030, with a considerable percentage presented at a late or advanced stage. It is paramount for the government to prioritise cancer reform to improve access to affordable cancer treatments.
Can we see the light at the end of the tunnel soon for all cancer patients with affordable treatments?
I am eagerly and urgently anticipating a positive answer to this.
Sew Boon Lui is a patient advocate and founding president of the Society for Cancer Advocacy and Awareness Kuching (SCAN). SCAN is a registered society and a Union for International Cancer Control (UICC) member. It was established to become the unified voice for all cancer patients to improve access to high-quality public health care and to create cancer awareness to the general public to increase survival.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.