MONTREAL, July 30 – The head of UNAIDS has recommended linking HIV/AIDS to broader rights-related movements to combat the criminalisation of sexual minorities and other vulnerable groups in Asia and the Pacific.
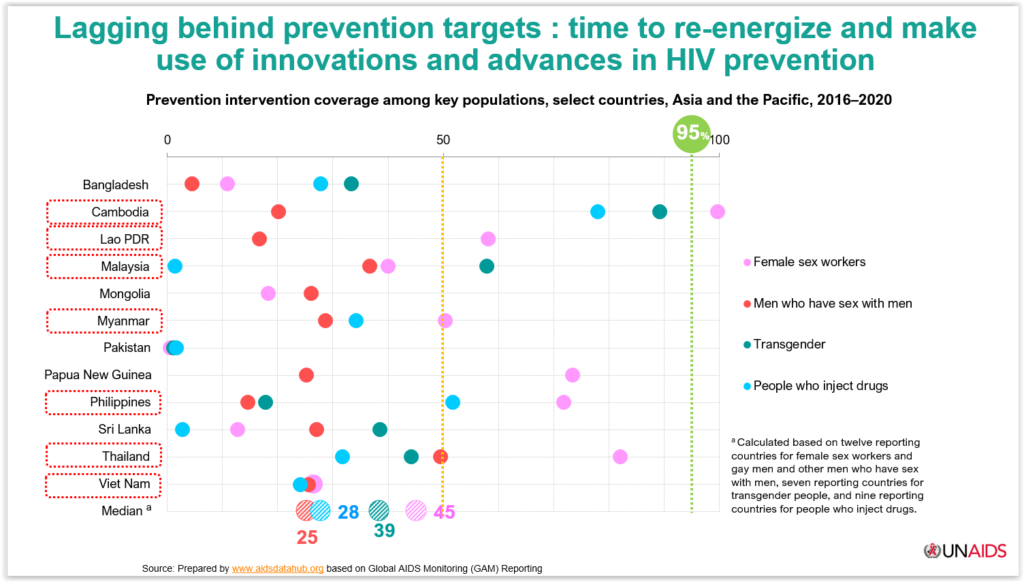
Winnie Byanyima, executive director of the United Nations agency, noted that new HIV infections in Asia are mostly affecting “key populations”.
Key populations are defined by UNAIDS as gay men and other men who have sex with men (MSM), sex workers, transgender people, people who inject drugs, and prisoners and other incarcerated people as the five main key population groups that are particularly vulnerable to HIV and frequently lack adequate access to services.
The UNAIDS Global AIDS Update 2022 report highlighted Malaysia and the Philippines as being among the countries with rising HIV epidemics among key populations, described as “alarming”.
From 2017 to 2021, Malaysia recorded the second highest proportion of new HIV infections among key populations in a sample of 11 countries at 78 per cent, behind the Philippines’ 93 per cent.
“What we know from our data, from our evidence, is that gay men and men who have sex with men and sex workers in many of those countries are criminalised and stigmatised. It drives them away from services,” Byanyima told a press conference Friday at the official opening of the 24th International AIDS Conference (AIDS 2022) in Montreal here.
“In some countries, they have punitive laws that come into force that when they want to get treatment, they risk getting arrested and being abused,” she added, in response to CodeBlue’s question on recommendations of HIV prevention measures for the lesbian, gay, bisexual, transgender and queer (LGBTQ) community in Malaysia.
Byanyima called for decriminalisation and to fight stigma and address social norms.
“We have to link HIV to the wider human rights movement, women’s rights movements, movements of gay men, to push against the attitude of society and to push against criminalisation.”
Health Minister Khairy Jamaluddin told Parliament last November that in 2021, about 63 per cent of reported HIV cases in Malaysia were linked to homosexual or bisexual relationships, and 33 per cent to heterosexual relationships.
From 2011 onwards, he said, Malaysia’s HIV epidemiology landscape shifted from the sharing of needles by people who use drugs to sexual transmission.
At the AIDS 2022 official opening press conference, International AIDS Society (IAS) president Dr Adeeba Kamarulzaman called for expansion of digital technology and HIV self-testing programmes.
“It’s important to address the social determinants of health,” she said.
Dr Adeeba, who is also an infectious disease physician and HIV/AIDS expert at Universiti Malaya, noted that HIV programmes led by key populations in Thailand, Cambodia, and Vietnam have been very successful.
In a presentation at a session on the World Health Organization’s (WHO) guidelines for key populations Friday, Dr Adeeba called for people-centred social innovation in HIV services.
These include a holistic examination of key populations’ needs, such as on HIV and other sexually transmitted infections (STIs), mental health, general health, and social support; a shift from a disease-focused to a people-centred approach by acknowledging key populations’ perspectives, experience and knowledge; and empowering key populations through a collaborative effort that involves key populations, health care workers, and caregivers jointly contributing to the process of prevention, diagnosis, and treatment.
She cited key population-led health services (KP-LHS) in Thailand that was an early adopter of innovations like pre-exposure prophylaxis (PrEP) medications that prevent HIV infection.
“Thailand has led the way in expanding PrEP,” Dr Adeeba said, adding that KP-LHS comprise more than half of HIV programmes in the country.
According to her presentation, seven KP-LHS organisations in Thailand are a “learning lab” for many innovations and new approaches in the HIV response, such as enhanced peer mobilisation, community-based HIV testing and antiretroviral therapy (ART), oral-fluids HIV screening and self-testing, and PrEP.
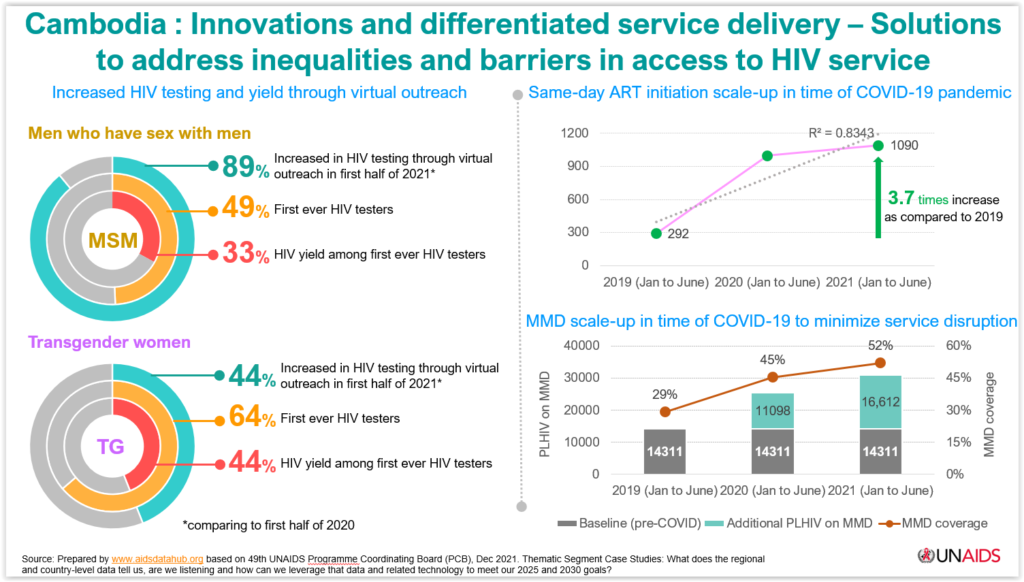
Cambodia has innovations and differentiated service delivery for solutions to address inequalities and barriers in access to HIV service, such as specific programmes for MSM and trans women.
Both programmes saw increased HIV testing and yield through virtual outreach.
The MSM and transgender women programmes in Cambodia reported 89 per cent and 44 per cent increase respectively in HIV testing through virtual outreach in the first half of 2021 compared to the same period in 2020.
HIV yield among first ever HIV testers was reported at 33 per cent in the MSM programme and 44 per cent in the trans women programme.
According to Dr Adeeba, Vietnam has partnerships between key populations and local governments in its HIV response.
“In my own country Malaysia, through Global Fund support, we have developed differentiated service delivery with strong partnership between the Malaysian AIDS Council and the Ministry of Health.”
She suggested expanding HIV services through self-testing, noting that this was commonly used for Covid-19 during the pandemic.
“We’re a very conservative country, but this forms some of the solutions to increase access to testing services for key populations,” Dr Adeeba said.
The infectious disease expert cited UNAIDS data that showed legal barriers to the HIV response remain in 38 countries in the Asia-Pacific. Thirty-six countries criminalise some aspect of sex work; 18 criminalise same-sex relations; 15 have laws that prohibit the possession of a certain limited amount of drugs for personal use; 21 criminalise the transmission of, non-disclosure of, or exposure to HIV transmission; and 14 restrict the entry, stay, and residence of people living with HIV.
“We need to do more and continue efforts to decriminalise not just sex work, but same sex relations and drugs,” Dr Adeeba said.








