KUALA LUMPUR, April 26 – The Ministry of Health (MOH) estimates 7,941 excess deaths in Malaysia during the past two years, just 2.4 per cent higher than expected based on historical trends from five years before the Covid-19 pandemic.
MOH’s estimate of 7,914 excess deaths from March 2020 to December 31, 2021, is not far off from the World Health Organization’s (WHO) projection of 7,692 excess deaths that was informed to Malaysia.
The 7,914 estimated excess deaths from any cause are about four times lower than the cumulative 31,462 Covid-19 fatalities officially reported by December 31, 2021.
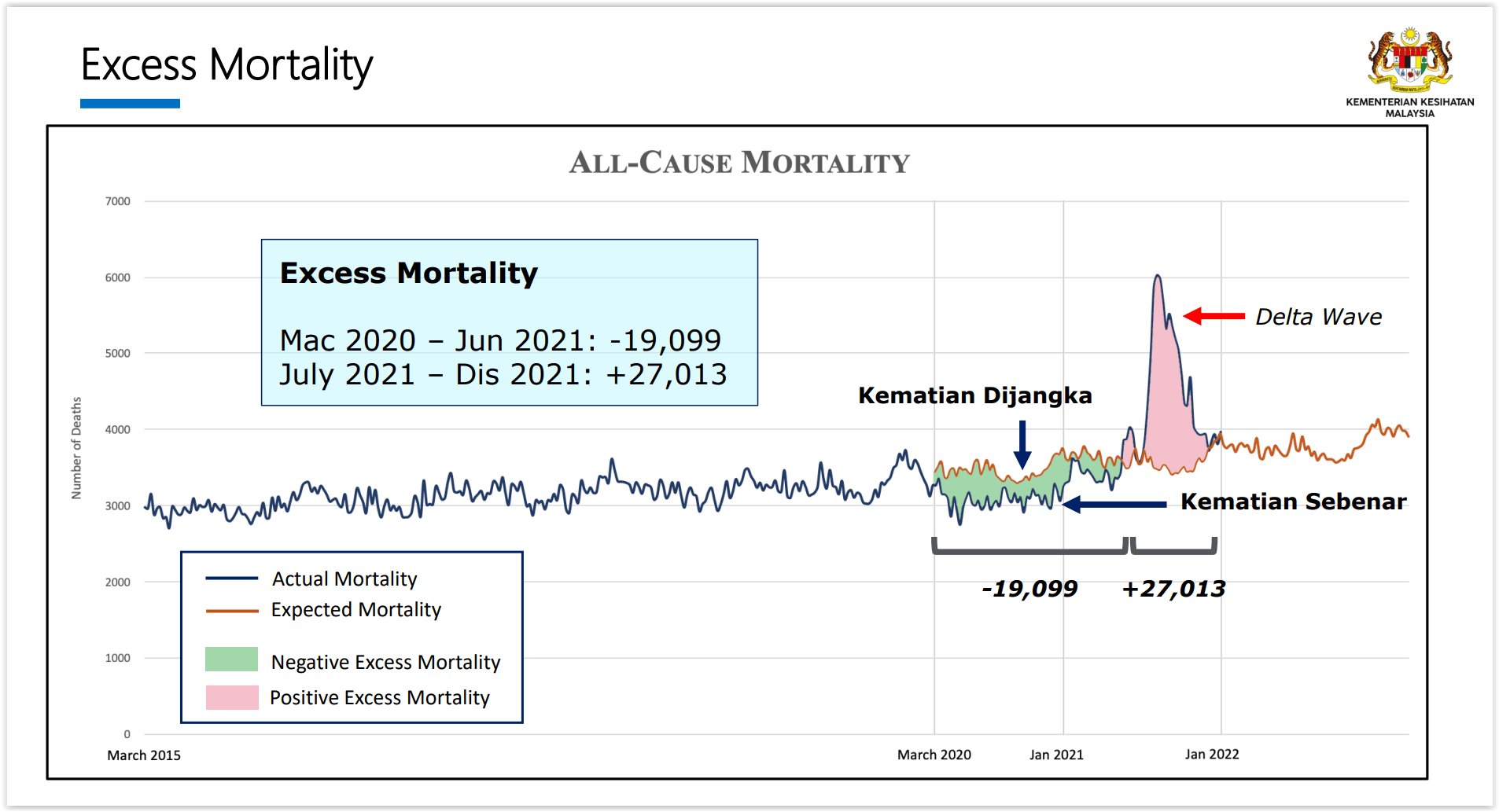
The much lower excess mortality projection compared to the official Covid-19 death toll is mainly due to the 19,099 fewer deaths estimated from March 2020 to June 2021, compared to the expected mortality trend based on pre-pandemic years from 2015 to 2019, known as negative excess mortality.
Excess mortality refers to how many more people died from any cause (or all-cause mortality) than would be expected based on historical trends before the Covid-19 pandemic. Negative excess mortality shows how many fewer people died than expected.
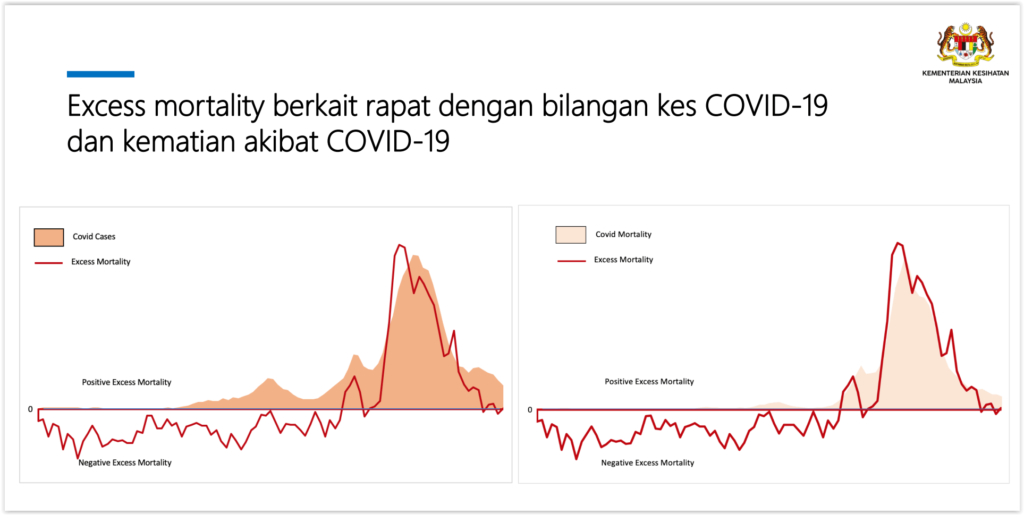
The study led by Dr Shubash Shander Ganapathy from the Institute for Public Health (IPH) estimated 27,013 excess deaths during the peak of the Delta variant wave in Malaysia between July and December 2021 – matching the reported Covid-19 mortality rate in that period.
Hence, Malaysia’s overall excess mortality during the past two years of the Covid-19 pandemic is just 7,914 estimated cases.
Malaysia officially reported 26,292 Covid-19 deaths from July 1 to December 31, 2021, which means that just 721 more deaths than the official coronavirus toll were estimated in that period, based on IPH’s model.
Lead researcher Dr Shubash said Malaysia’s negative excess mortality during the earlier phase of the pandemic can be attributed to reduced deaths due to cardiovascular diseases, chronic respiratory diseases, and pneumonia, as shown in an earlier analysis.
“So, we believe these reductions have come – now again, we can only theorise this because we can’t actually say why this has happened for sure – but we theorise that this is the changes in lifestyle that occurred among the people during the pandemic,” Dr Shubash told a media briefing yesterday.
“As we know, [during the] lockdown, people were spending more time at home, their food intake, and their habits would have also changed – but this obviously had a positive effect on the overall population.
“Now, excess mortality has its pros and cons. Maybe one of its cons is probably it doesn’t say exactly why, but the good thing is it takes the population as a whole as an overall effect is seen by excess mortality.
“This gives us an idea that overall, for the whole of the pandemic, we did have less deaths that have occurred.”
Contrary to Dr Shubash’s theory about healthier lifestyles during the pandemic leading to negative excess mortality, a cardiologist previously pointed out in May 2021 that lockdowns led to sedentary lifestyles and weight gain among some due to the shutdown of outdoor physical activities and higher consumption of unhealthy fast food from food delivery. An increase in diabetes and heart disease cases was also projected due to the disruption of diagnosis and treatment during the pandemic.
Crucially, the potential effect of late registration of deaths and backlogged reporting of Covid-19 mortality during the pandemic on IPH’s model was not mentioned. A March 2021 presentation by a Department of Statistics Malaysia (DOSM) on the disruption of civil registration and vital statistics in Malaysia due to Covid-19 stated that deaths were reported by the heir, for the purpose of getting the death certificate, to the National Registration Department (NRD) — data used by IPH’s model — within 90 days of the death during the Covid-19 pandemic, as opposed to the conventional process of seven days.
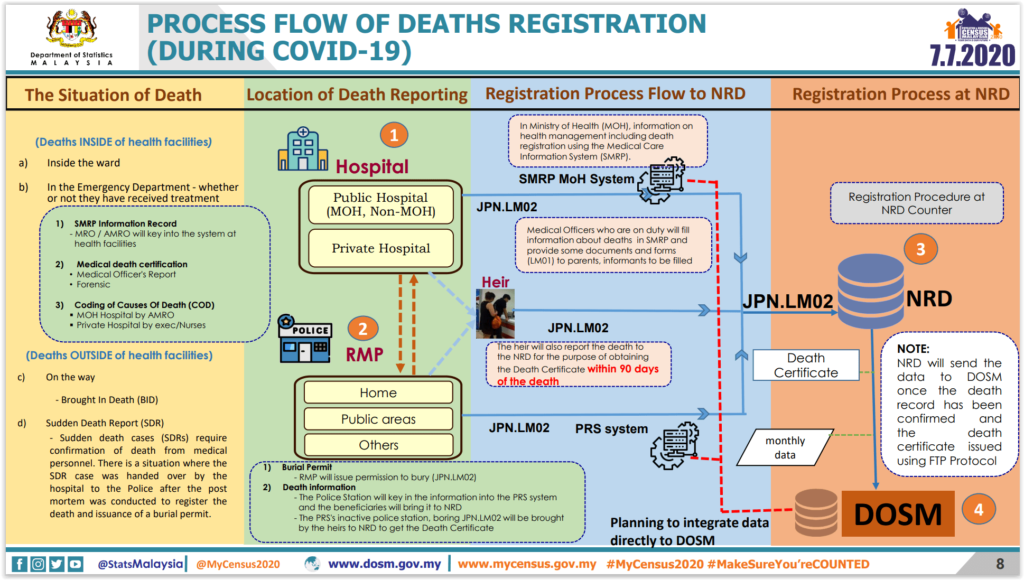
DOSM pointed out that the declining trend of births, deaths, and non-Muslim marriage and divorce during Covid-19 was due to late registration. DOSM also said that NRD counters for birth and death registration were closed from mid-March to mid-May 2020, and later only available by appointment.
IPH’s modeling that matched high excess mortality to Covid-19 deaths during the Delta wave also appeared to rely on the reported Covid-19 mortality trend in the period, without accounting for backlogged Covid-19 death reporting previously acknowledged by MOH itself. Health Minister Khairy Jamaluddin said last September that brought-in-dead cases could take up to six weeks for confirmation as Covid-19 death, noting that the massive backlog in overall Covid-19 death reporting was due to the surge of infections in the Klang Valley in July and August.
Also present during yesterday’s briefing were Health director-general Dr Noor Hisham Abdullah and Institute for Clinical Research (ICR) director Dr Kalaiarasu Peariasamy.
Dr Noor Hisham said the country’s negative excess mortality of -19,099 between March 2020 and June 2021 is proof that preventive public health measures, such as face mask wearing and high compliance to health protocols, can keep mortality rates low.
Malaysia’s cumulative Covid-19 death toll per capita as of April 24 is the highest in Asean and among the highest in Asia, based on data from Our World In Data, though India, Indonesia, and the Philippines are likely under-reporting coronavirus-related mortality.
More Malays, Fewer Chinese and Indians Estimated To Die Than Pre-Pandemic Years
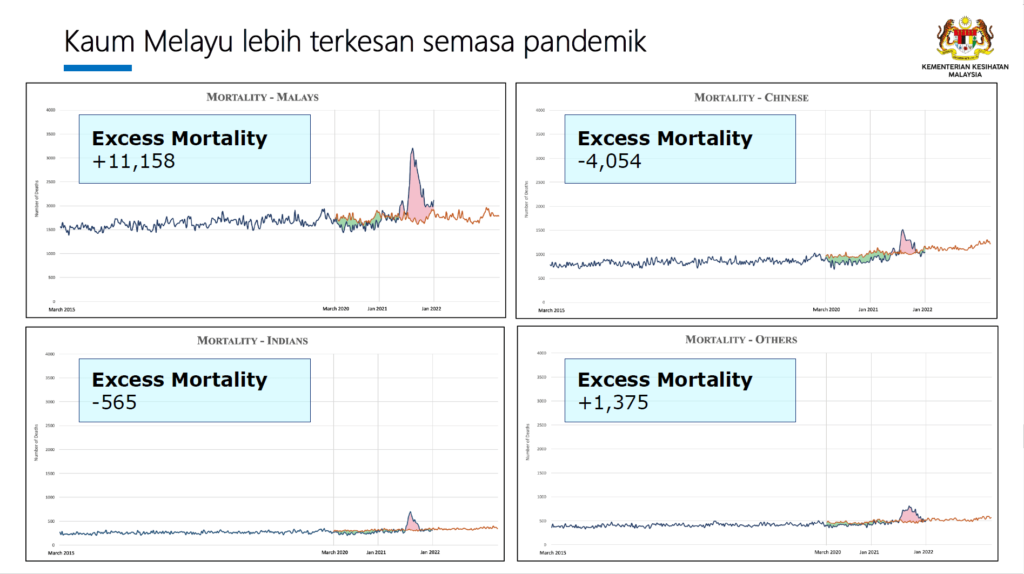
By ethnic group, Malays were likely to be most affected during the pandemic with 11,158 excess deaths estimated, compared to a negative excess mortality of -4,054 cases among the ethnic Chinese.
This means that more Malays but fewer Chinese were estimated to die than would be expected based on pre-pandemic historical trends.
Excess mortality among ethnic Indians was projected at -565 deaths, indicating that fewer of the community are estimated to have died during the pandemic compared to pre-pandemic historical patterns.
MOH estimated 1,375 excess deaths during the pandemic among other ethnicities.
The study attributed the ethnic Chinese community’s projected negative excess mortality to lower risks for non-communicable diseases like diabetes, hypertension, high cholesterol, and obesity compared to other ethnic groups; healthier lifestyles; and overall higher compliance of 3W (wash hands, wear a mask, watch your distance) practices.
Health literacy was also higher among the ethnic Chinese at 36.6 per cent, compared to 30.6 per cent among Malays and 30.3 per cent among ethnic Indians, MOH said, citing the National Health and Morbidity Survey 2019.
More Men, Those Aged Above 40 Estimated To Die Than Pre-Pandemic Years
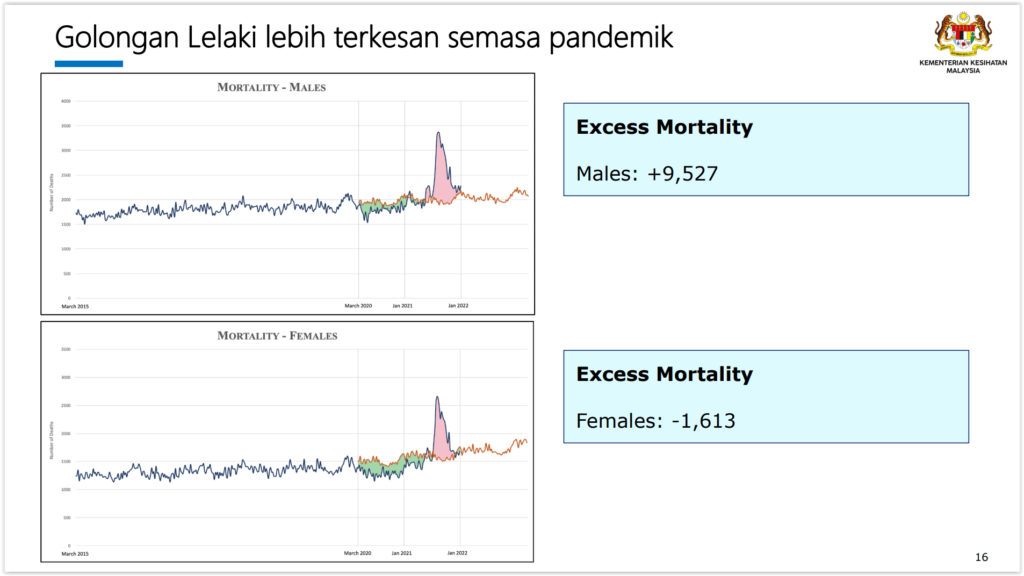
By gender, males were projected to be more affected during the pandemic with 9,527 estimated excess deaths, versus negative excess mortality of -1,613 excess deaths in females.
This indicates that more men, but fewer women, were estimated to die in the past two years compared to pre-pandemic years.
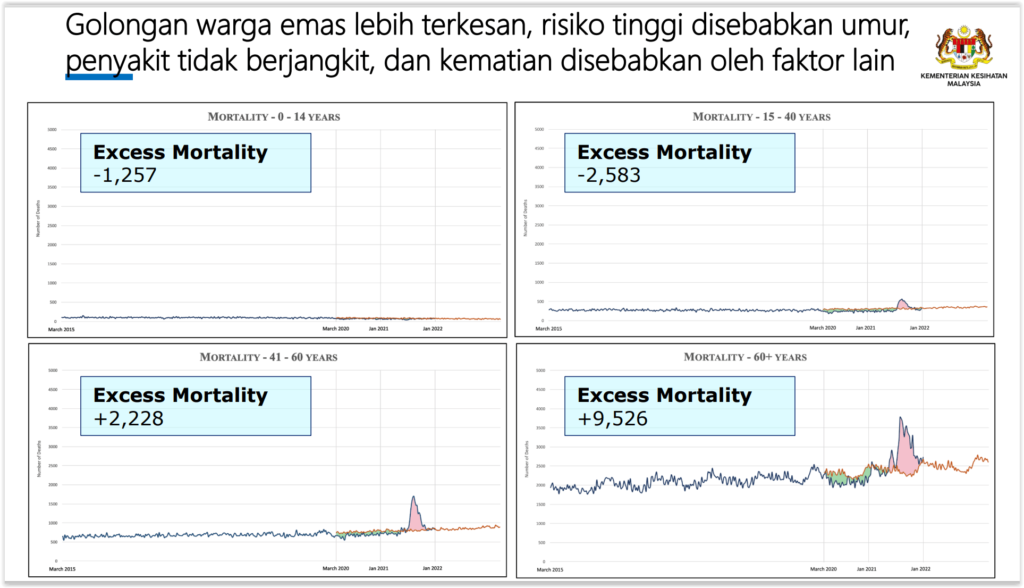
By age, excess mortality was highest among individuals aged 60 years and older with 9,526 excess deaths in the past two years of the pandemic, followed by individuals aged 41 to 60 (2,228 excess deaths).
Negative excess mortality was estimated among those aged 15 to 40 at -2,583, while those aged 14 years and younger were -1,257.
This shows that fewer people aged 40 and younger were estimated to die during the pandemic than expected based on pre-pandemic trends, but more deaths were estimated among older people than predicted. Covid-19 generally is more brutal towards the elderly.
By registration, estimated excess mortality related to deaths in hospital accounted for 53 per cent of the total 7,914 estimated excess deaths at 4,151 cases, while estimated deaths that occurred outside of health facilities contributed to 3,763 cases, or 47 per cent of excess mortality. The proportion is similar to pre-pandemic figures.
IHME Model Doesn’t Explain Influence of Factors
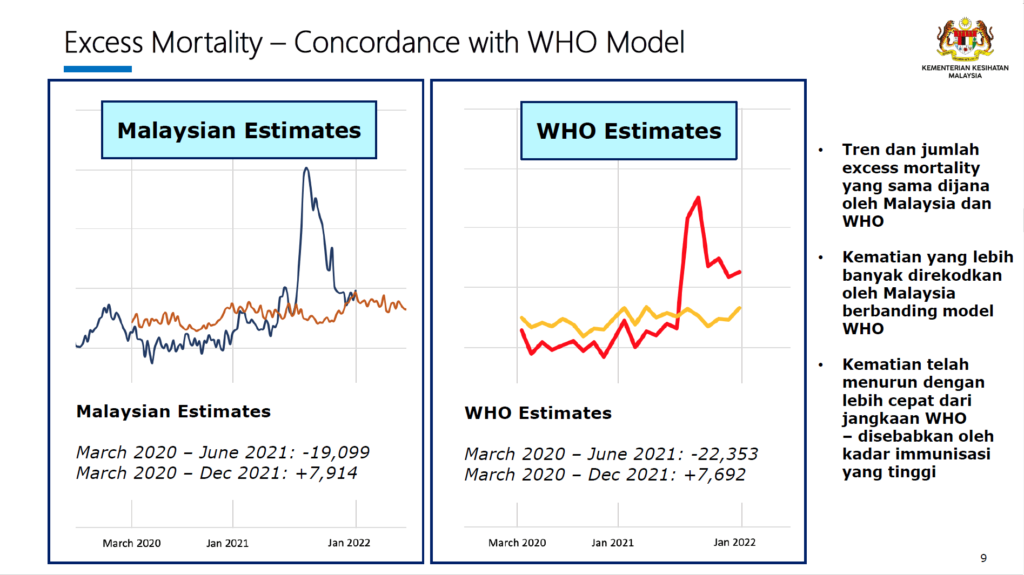
Local mortality data from the NRD and hospital admission records from MOH’s Health Informatics Centre from 2015 to 2021 were sourced for the IPH study. The WHO’s projection, on the other hand, conducts mathematical modelling utilising a different set of indicators and variables that occurred during the pandemic, said Dr Shubash.
Early estimates by the WHO for Malaysia were obtained through direct consultation as the figures have yet to be released globally.
“The important factor in the data produced by the WHO and Malaysia is the similarity in trend. The trend is almost similar which verifies the two models used,” Dr Shubash said.
“This is different from the model used by the Institute for Health Metrics and Evaluation (IHME). The IHME reports excess mortality in totality up until the end of 2021. Now, although they provided a list of factors and data [involved in their modelling], they did not provide an explanation on how these factors influence the model.
“So, it makes it difficult for us to make a good appraisal on how their model is different from ours,” Dr Shubash said.
Additionally, Dr Shubash said the model by the IHME from the United States’ Washington University failed to report their figures on a weekly and monthly basis, which is needed to analyse trends for excess mortality.
“When we analyse and interpret the findings of excess mortality, the trend is important as it explains why the figures go up or down. So, when the IHME doesn’t explain or provide the necessary data for us to determine the trend, it becomes hard for us to point out where the discrepancies are.
“We will definitely get in touch with IHME to get further data so that we can correct our model and learn from them, or we get them to correct their model, which not only affects us but the model for other countries as well,” Dr Shubash said.
The Covid-19 excess mortality team from IHME previously estimated 48,100 excess deaths in Malaysia from January 2020 to December 2021, which is 1.5 times higher and 16,600 more deaths than the 31,500 Covid deaths officially reported in that period.
IHME researchers estimated that 18.2 million people died globally because of the Covid-19 pandemic in the last two years, as measured by excess mortality, three times higher than the official record of 5.94 million deaths due to Covid-19.
IHME attributed the huge difference to Covid-19 underdiagnosis due to insufficient testing, reporting challenges, or higher than expected mortality from other diseases due to pandemic-related changes in behaviours or reduced access to health care or other essential services.
Dr Shubash acknowledged that MOH’s excess mortality projection may have missed certain Covid-19 deaths, though he estimates the missing figure to be minimal as greater omissions would have resulted in multiple spikes and reflected in the ministry’s modelling.
He also said Malaysia’s locally estimated excess mortality of 1.32 per cent from March 2020 to September 2021 was better than countries like the United States (18.62 per cent), Britain (13.84 per cent), the Philippines (19.11 per cent), or Thailand (5.01 per cent), citing figures from The Economist’s model.
The Economist projected negative excess mortality for New Zealand, Australia, Singapore, and Japan, which means that these countries reported lower deaths during the pandemic than expected based on pre-pandemic mortality data.