Businesses, golf courses and schools are now open, and from October 11, crossing state borders is allowed, marking the day we finally return to a ‘normal’ state. Well, not quite normal, since we are merely transitioning to the endemic phase of the pandemic, a coveted status for countries able to vaccinate a large proportion of its population.
We have just hit 90 per cent adult vaccination rate, a remarkable achievement by our government, which has put us in this privileged category. But it does not mean the worst is over (see what happened in Singapore, Israel, and Iceland, all highly vaccinated countries experiencing resurgences of Covid-19, due to the Delta variant).
It just means from now on we are going to let it be. All Malaysians will become infected eventually (already a huge proportion have been), and we just have to learn to live with it, like we do with other endemic infectious diseases in Malaysia, notably dengue and flu.
But how do we do this? First, an accounting of our recent past.
The Darkest Episode In Malaysian History
As disasters go, our country has just been through the darkest episode of its history.
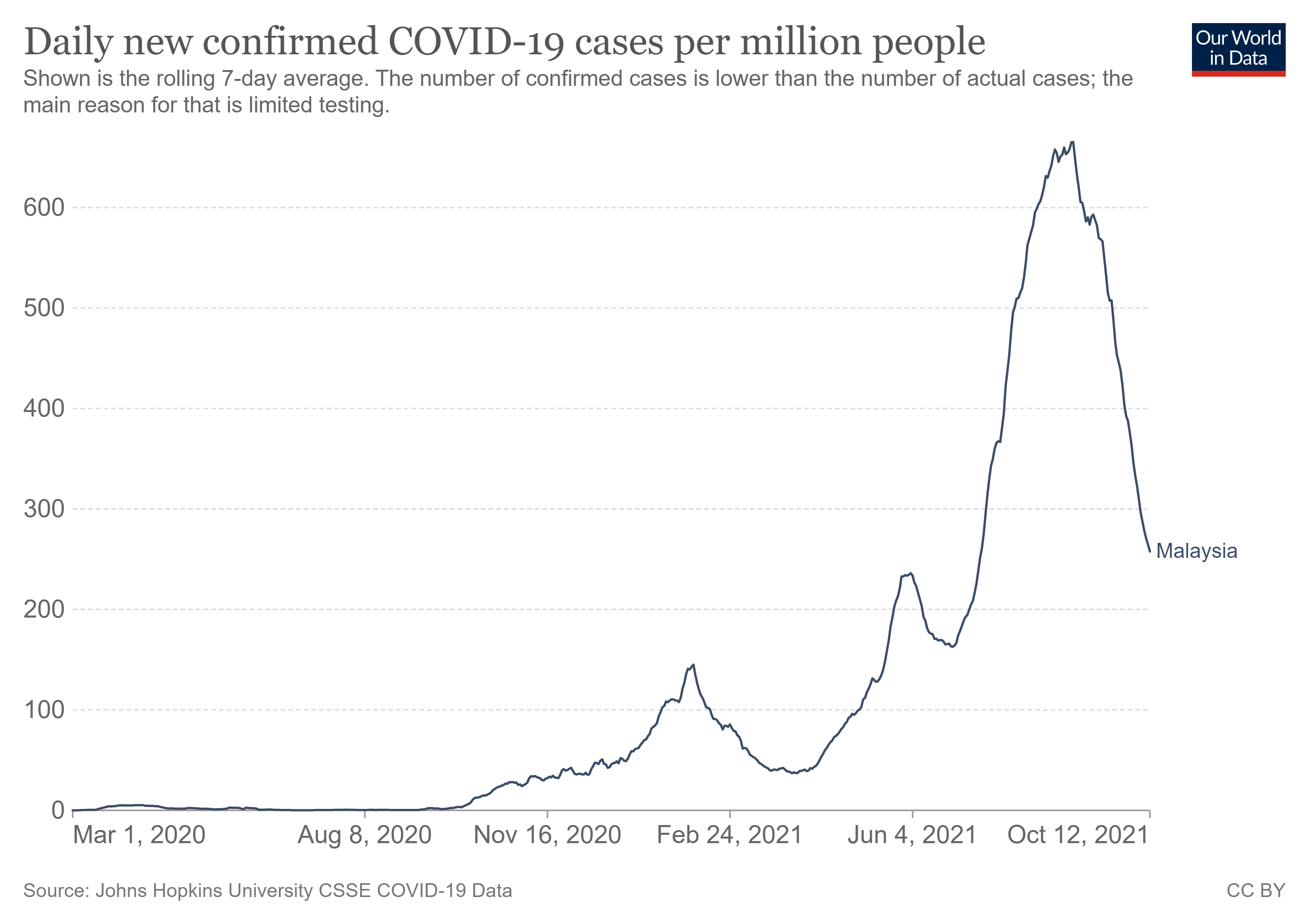
The current wave of Covid-19 started in mid-April 2021, and a lockdown was imposed on May 6. The wave peaked on August 26 with 24,599 new cases recorded on that day.
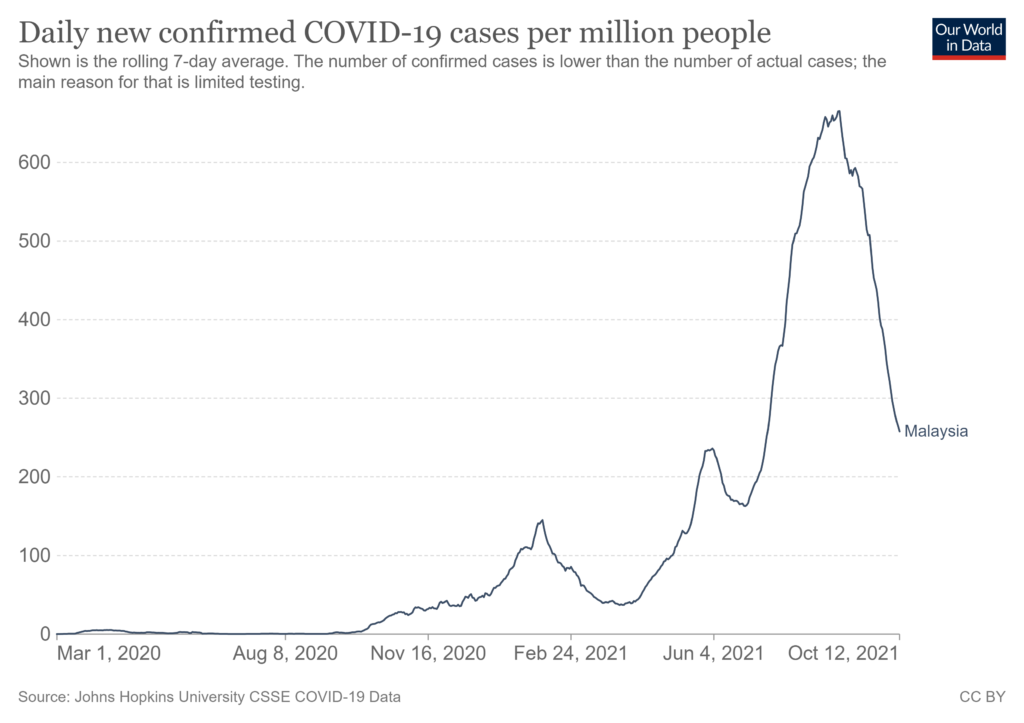
By October 7, 2.31 million Malaysians have been infected, and 27,113 have died of Covid-19.
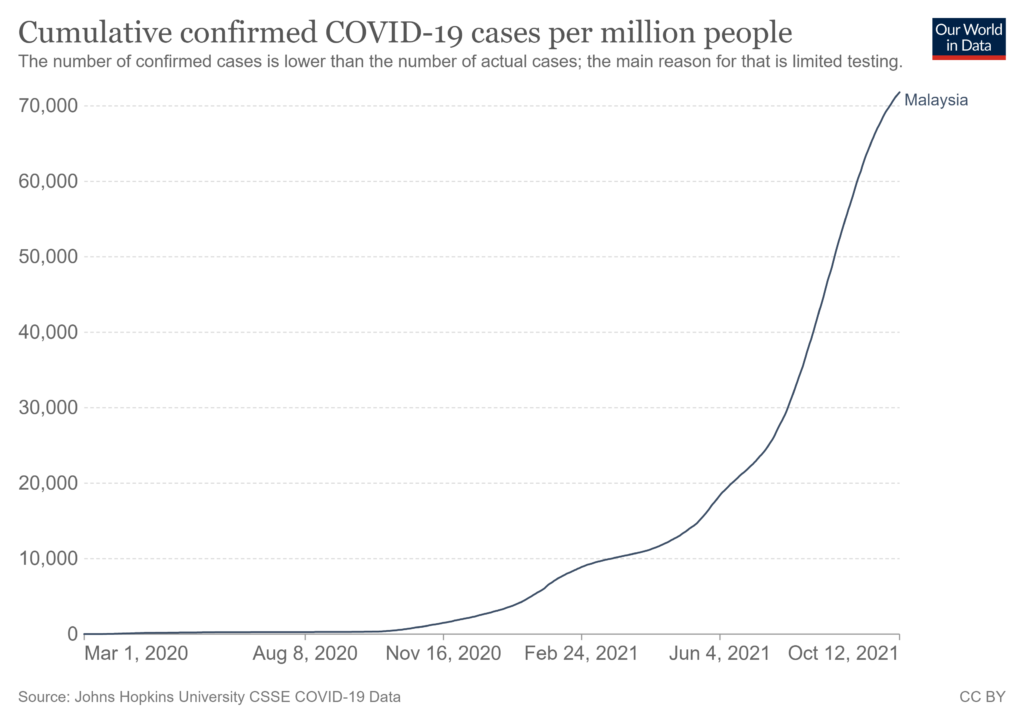
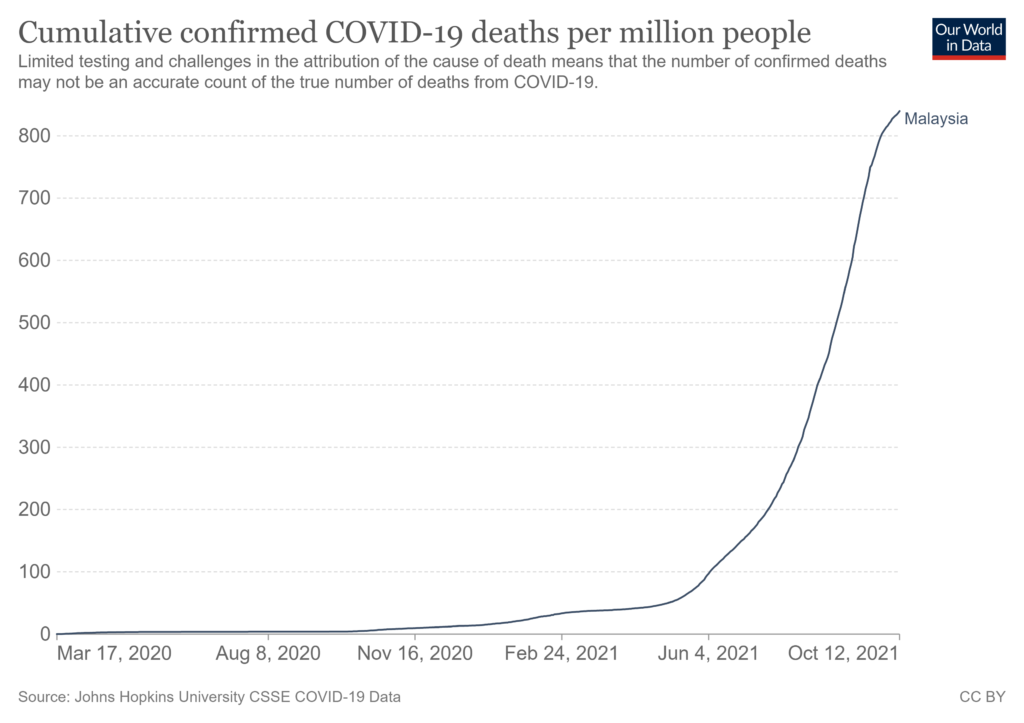
Over the course of six months from April to October, Malaysia emerged as one of the most heavily affected countries in the world. In terms of both number of cases and death rate, we beat all our neighbours by a long stretch.
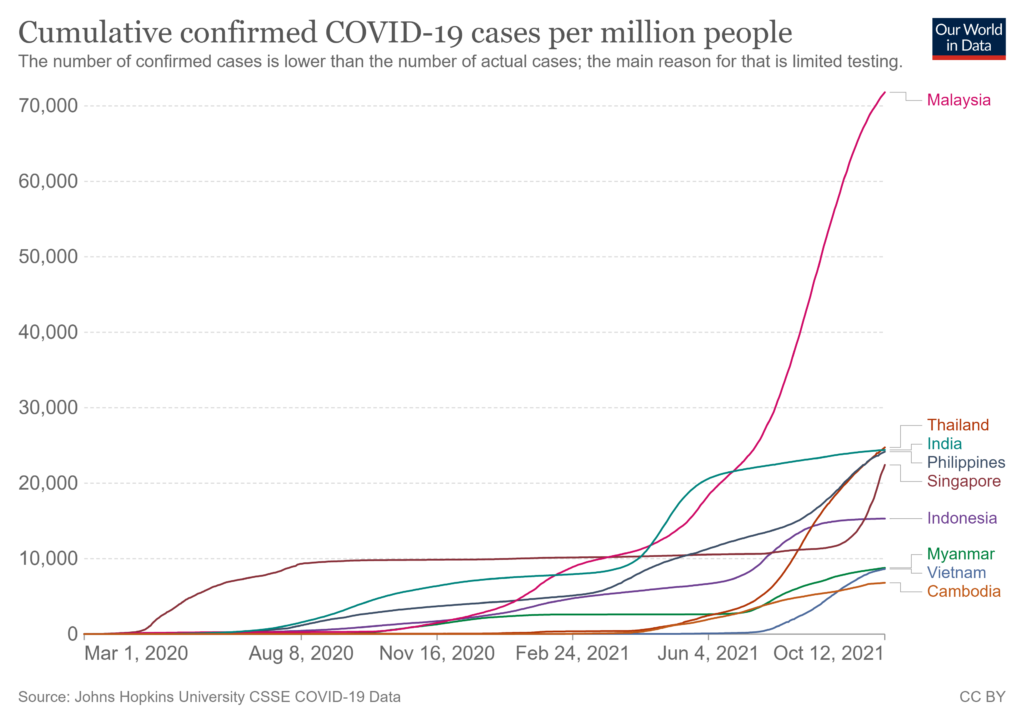
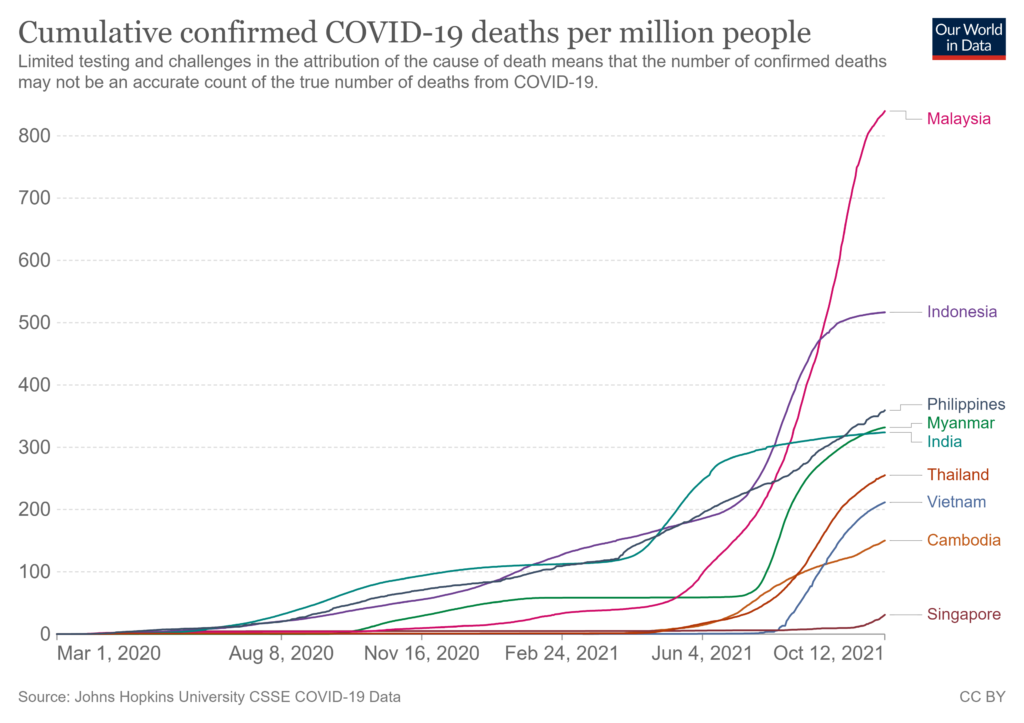
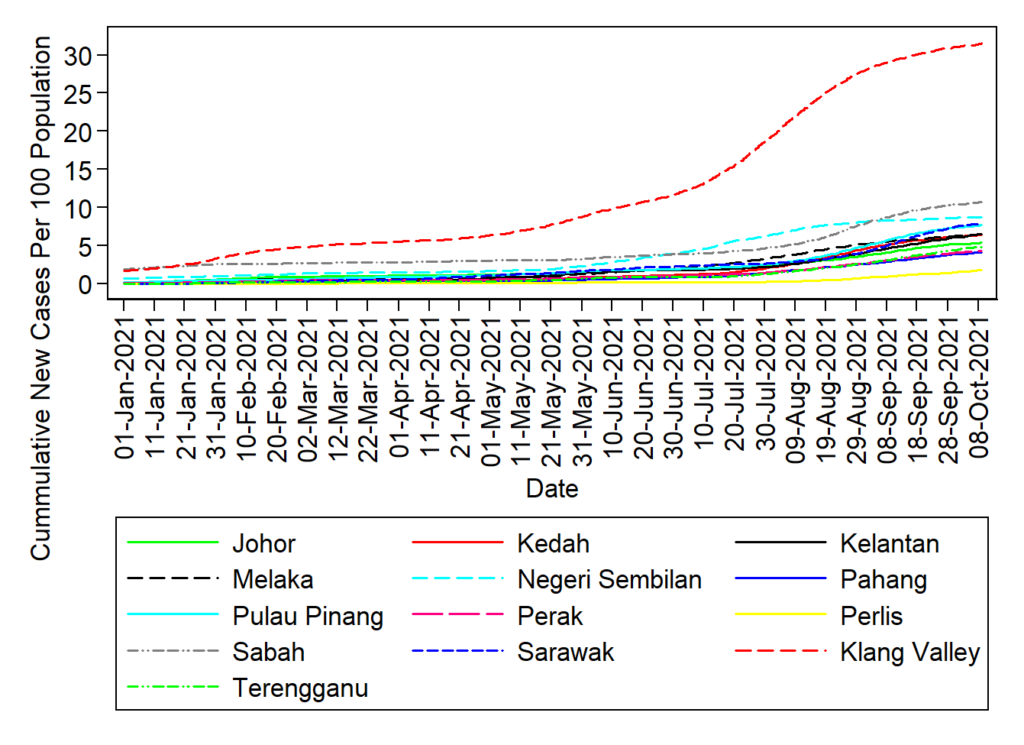
Measured in percentage of people infected, the Klang Valley exceeded 30 per cent by October. This is just counting those who have been tested positive. Including people who were infected but not tested, my guess is more than 80 per cent of people have been infected within the Klang Valley. The rest of the country will no doubt catch up. Do note the huge surge in infections occurred in the last six months when the country was under lockdown.
Covid-19 has hit us hard, which is painful for a country which has not experienced famine, war, civil strife or major natural catastrophes in the past 50 years.
Will our recent tragic experience recur, despite all of us all being vaccinated? The answer is both yes and no.
Yes, because vaccine-induced immunity will wane over time. We do know that antibodies (specifically neutralising antibodies which block virus entry into our cells) do wane over time, but the other two components of our immune response (the so-called memory B and T cell responses) may hold up longer.
New virus variants will emerge and some may escape vaccine-induced immunity. The current vaccines are holding up well against the Delta variant; it no longer prevents vaccinated people from becoming infected and transmitting the virus, but it still protects us from severe disease.
We will continue to experience outbreaks of Covid19 here and there, but not on the same nationwide scale as the one we just had in the last six months.
A booster vaccine dose, which I am certain the government will introduce only for select groups, will likely help. This is how endemic Covid-19 is; every year, several thousand people will die of it, the same way dengue affects and kills the same number of people.
How Do We Live With Covid19 Safely?
Regardless of the outcome, which remains uncertain, there are plenty that we can do to live with Covid-19 safely, and I don’t mean more lockdowns, whether self-imposed or otherwise.
1. Vaccination
Firstly, get yourself and everybody around you vaccinated. Now that we are in the endemic phase, you will meet the airborne virus sooner or later.
Vaccination has become even more important because it will protect you from severe disease. You will want to meet the virus from a position of strength, which means only after you are fully vaccinated.
Having everyone vaccinated actually helps protect against the emergence of variants. Variants emerge because there are large pockets of unvaccinated people within a population, in whom the virus transmits more freely, stays in hosts longer, and causes more severe disease. For all these reasons, the emergence of more new variants is likely.
Now that you are vaccinated, while your immunity may be waning, you are still protected against severe disease. It is probably a good time to catch the virus, which will further boost your immunity.
The problem is you don’t know whether you are personally protected, since vaccines are not 100 per cent effective). The best readily available measure which correlates with immune protection is the neutralising antibody (Nab) level.
If your Nab level is low, you may want to consider getting yourself a booster dose soon, than wait for the government’s decision on this. Do note that a government makes decisions for the entire population, and the risk-benefit calculus is not necessarily the same as one you would apply for yourself.
Remember, it is okay (and even desirable) to be infected by the virus, but only while you still have immunity.
2. Three Ws And Three Cs
Secondly, you must continue to observe the well-known three Ws and three Cs. Notice that I have added wash your nose to the usual advice to wash one’s hands. It helps if more of us understand the scientific rationale behind the three Ws and three Cs.
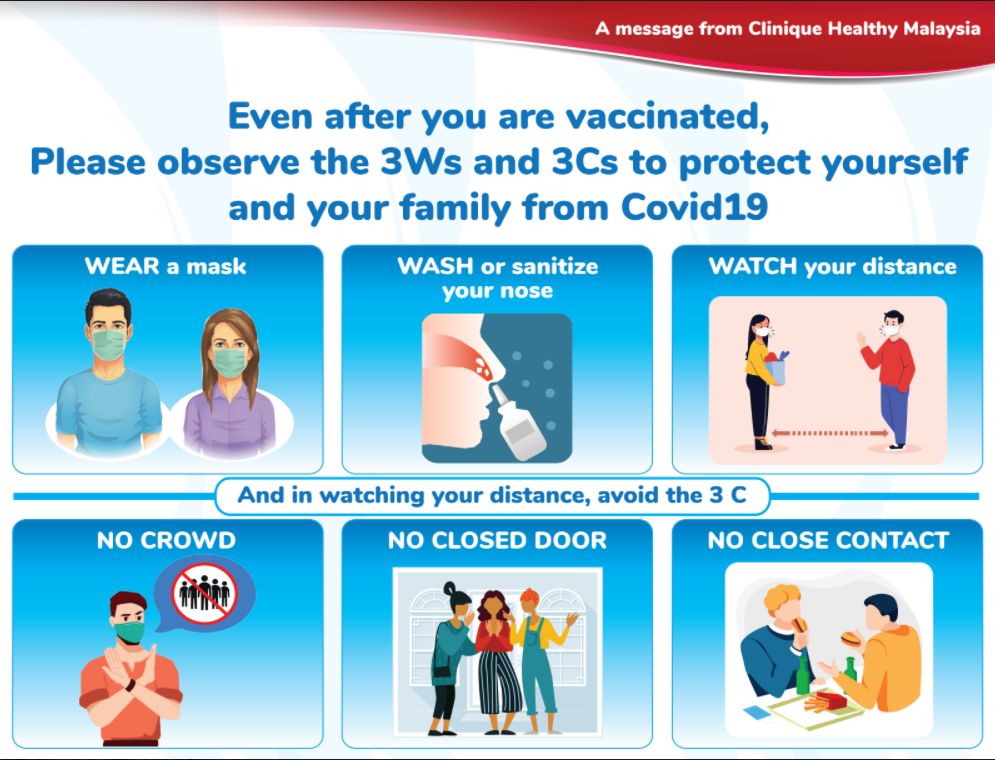
The Covid-19 virus spreads through the air you breathe in, and not through your hands after touching a surface contaminated by the virus (a year ago we used to believe that, hence the past emphasis on hand washing, sanitising surfaces, etc.).
When an infectious person talks, coughs, sneezes, he discharges virus particles which are carried in the air in two forms, namely droplets and aerosols (<5 um in size).
Droplets are heavy and drop to the ground quickly (and contaminate surfaces). This is why we should wear masks, keep our distance (one to two metres apart), and practise hand and surface sanitisation.
But aerosols, being very light, can be carried in the air for a long time over a long distance, and in a poorly ventilated indoor space, they can recirculate, to be inhaled by all present.
Masking, distancing and handwashing do not protect you from virus-laden aerosol. Using nasal sprays and proper ventilation of crowded indoor spaces will.
3. Screening Tests
A congregate setting is where a large number of people must unavoidably meet or interact for a prolonged duration (several hours), and often, repeatedly.
Examples are workplaces, schools, dormitories, and nursing homes. Such settings are well known for Covid-19 transmission, since many outbreaks in Malaysia occurred in workplaces.
Owners or managers of such places should consider screening tests for all persons before entry. At Parliament, which opened recently, Members of Parliament and Senators are tested before entry, and many schools are already doing this. Even some high-end restaurants require this of their customers for indoor dining.
RTK antigen tests are most commonly deployed for this purpose. Its low cost and ease of use makes it suitable for this, despite its low sensitivity, which can be mitigated by more frequent testing to enable detection of an infected person, as his viral load increases over time.
Ideally, this should be twice weekly; the Ministry of International Trade and industry requirement to test once every two weeks is more symbolic than science-based. More sensitive, but more costly, screening tests are also becoming available.
4. Indoor Space and Ventilation
Indoor activities are unavoidable because not everything can be conducted outside (classroom learning, indoor sports, offices, factory floors, etc.). We are also driven indoors by our desire for comfort in our tropical climate.
Safe use of indoor spaces where many other people are present requires monitoring the CO2 of indoor air (humans take in oxygen and exhale CO2, which, in a poorly ventilated room, will quickly accumulate).
A safe level is less than 800 ppm or lower. If possible, keep windows open and have a window fan on, especially when CO2 is more than 800 ppm.
Air purifiers (with HEPA filters) will also help to improve indoor air quality. For very high-risk indoor spaces, its safe use requires monitoring indoor air for the Covid-19 virus, and users should test negative before entry.
In summary, to stay safe while we learn to live with Covid-19, do get jabbed and do continue to observe the three Ws and three Cs. Going about your daily life, whether at work or play, will get you indoors with other people, so do pay attention to air ventilation.
It would be ideal too if others around you are all tested negative before entry. It is okay to be exposed to the virus, but not too much.
Avoiding Covid-19 at all costs is not necessarily the best protection, nor is it compatible with a normal life.
References
Rustom Antia, M. Elizabeth Halloran. Transition to endemicity: Understanding COVID-19 Immunity (IF31.745), Pub Date : 2021-09-24, DOI: 10.1016/j.immuni.2021.09.019
Larremore DB et al., Test sensitivity is secondary to frequency and turnaround time for COVID-19 screening Sci. Adv. 10.1126/sciadv.abd5393 (2020)
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.