KUALA LUMPUR, May 8 — Doctors and health care workers across public and private sectors said they have had insufficient personal protective equipment (PPE) amid the Covid-19 crisis, a survey revealed.
According to the online survey by Malaysian doctors Dr Timothy Cheng, Dr Nur Asyikin Mohd Yunus, Dr Imran Idris, Dr Khairil Idham Ismail, and Dr Amar-Singh HSS — which polled 788 health care workers from April 13 to 19 — this problem was more pronounced in private clinics and hospitals at 83 per cent; followed by 77 per cent in Ministry of Health (MOH) hospitals; 69 per cent in state health departments, district health offices, and public health clinics (Klinik Kesihatan); and 53 per cent in public university hospitals.
The survey, sent to CodeBlue, also found that nearly half, or 41 per cent of respondents, did not feel adequately protected by PPE against the risk of coronavirus transmission in their workplace.
Health care workers at state health departments, district health offices, and public health clinics felt the safest with the level of their protective gear at 71 per cent, followed by 59 per cent of respondents at university hospitals, 57 per cent at MOH hospitals, and 43 per cent at private clinics and hospitals.
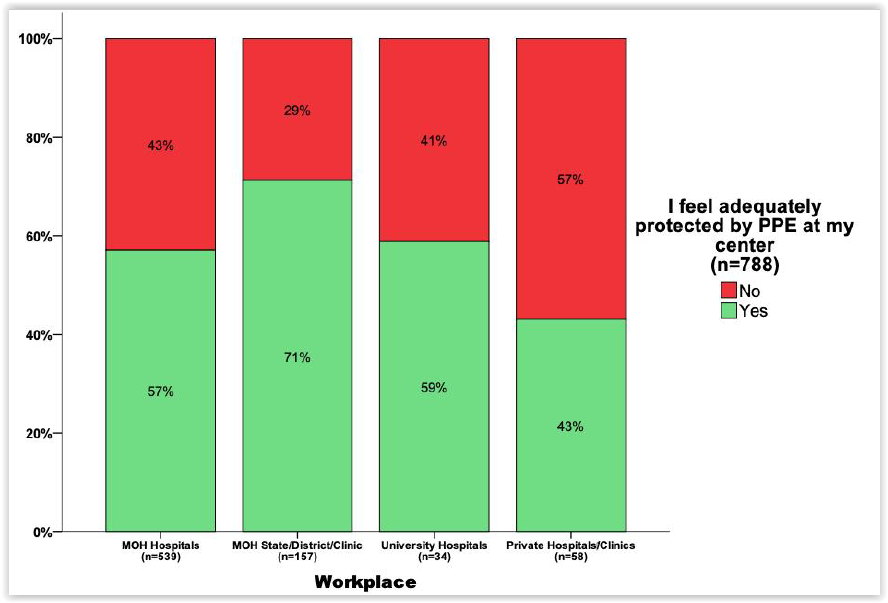
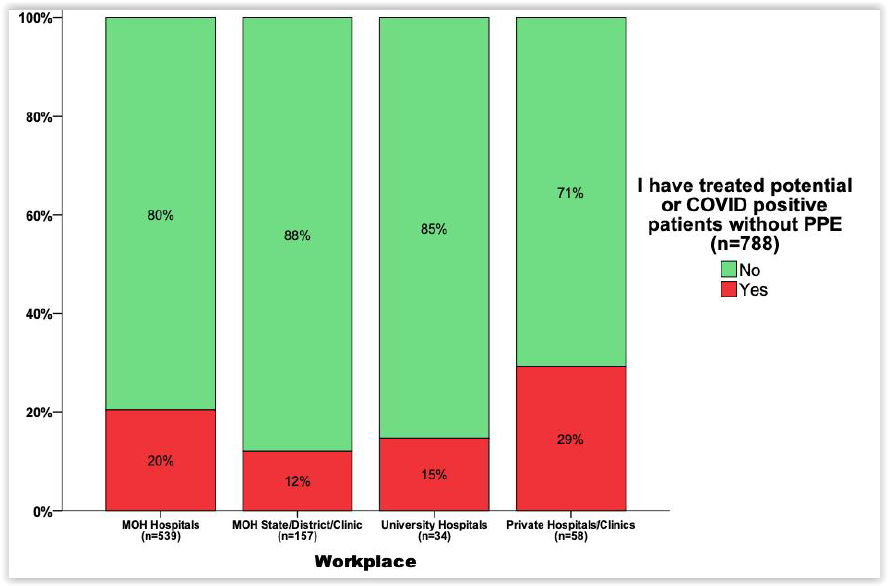
Although 53 per cent of respondents from all MOH facilities (hospitals and clinics) stated that they felt adequately protected at their centre, 16 per cent from those facilities indicated that they had treated potential or Covid-19 positive patients without sufficient PPE.
Some 59 per cent of respondents from university hospitals believed they had sufficient protection in their workplace, but 15 per cent said they have treated possible or confirmed coronavirus patients without sufficient protective gear.
Less than half, or 43 per cent, of respondents from private clinics or hospitals felt adequately protected at their centre, while 29 per cent said they have treated possible or confirmed coronavirus patients without sufficient protective gear.
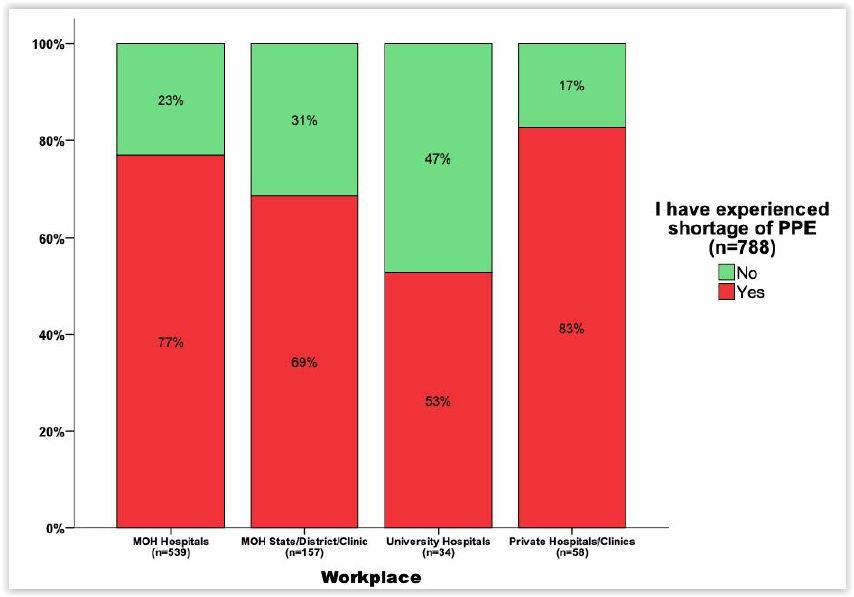
As of April 23, the survey authors noted, 325 Malaysian health care workers have been infected with Covid-19, accounting for 5.8 per cent of the country’s cumulative cases.
“It is still unclear regarding mode of transmission for ~ 30 per cent of these cases and it is worrying that the number has doubled in three weeks,” they said.
“No one is spared from the risk of infection, be it the frontliners who handle screening of potential Covid-19 patients; HCW (health care workers) in Covid-19 wards or other areas of the hospital. Transmission can occur from asymptomatic/undetected patients or between HCW.”
MOH has repeatedly insisted that none of its health care workers contracted Covid-19 from managing coronavirus patients in Covid-19 wards or the intensive care unit (ICU), but paediatricians Dr Musa Mohd Nordin and Dr Zulkifli Ismail said hospital-acquired infections should cover infections acquired within hospital facilities, whether it is from the pantry or from coworkers.
According to the survey, the majority of health care workers from MOH hospitals (58 per cent) and private hospitals or clinics (52 per cent) reported using DIY protective clothing; as well as 48 per cent among state health departments, district health offices, or government clinics; and 15 per cent in university hospitals.
The usage of DIY PPE was more common in East Malaysia at 64 per cent, compared to 45 per cent in the peninsula.
Survey authors raised concerns about whether self-made PPE were of acceptable quality, highlighting the “methods of production, types of materials used, measurements and suitability of usage in different areas of risks”.
“Concerns were also raised by some of the respondents on this issue via comments given in the comment boxes ‘DIY PPE among staffs have resulted in extra burden’, expressing their grievance of having to make their own PPE which added to their already burdensome clinical duties,” they said.
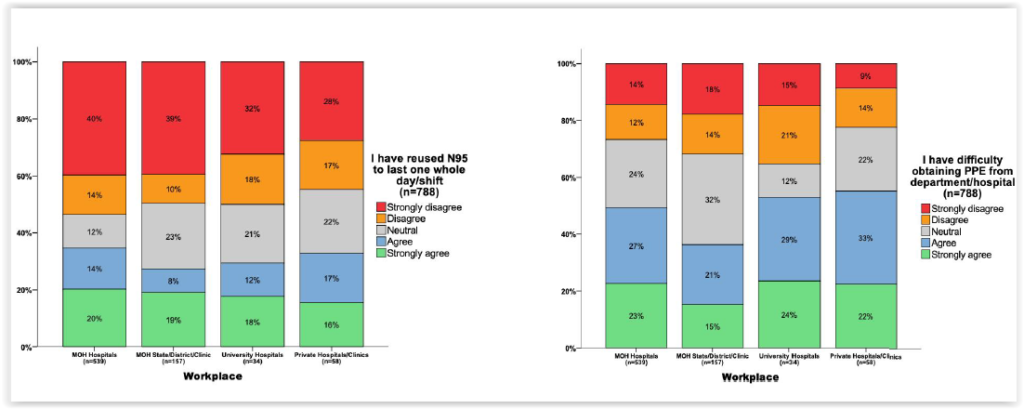
According to the survey, about a third (33 per cent) of health care workers from private clinics and hospitals said they reused N95 respirators, followed by 32 per cent at MOH hospitals and clinics, and 30 per cent at university hospitals.
“Although permissible, this practice increases the risk of infection of pathogens to the HCW and should be avoided if possible,” survey authors said.
More than half, or 55 per cent, of respondents in private medical facilities claimed difficulty in obtaining PPE from their department or facility, followed by 53 per cent in university hospitals and 47 per cent in MOH hospitals and clinics.
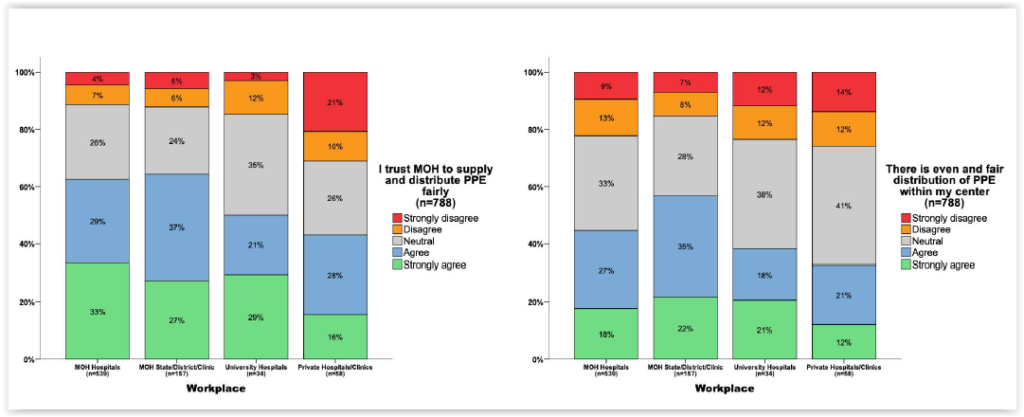
Between 44 per cent and 64 per cent of health care workers across public and private facilities said they trusted MOH to supply and distribute PPE fairly. However, only between 33 per cent and 57 per cent of respondents across the board said protective gear distribution within their centre was even and fair.
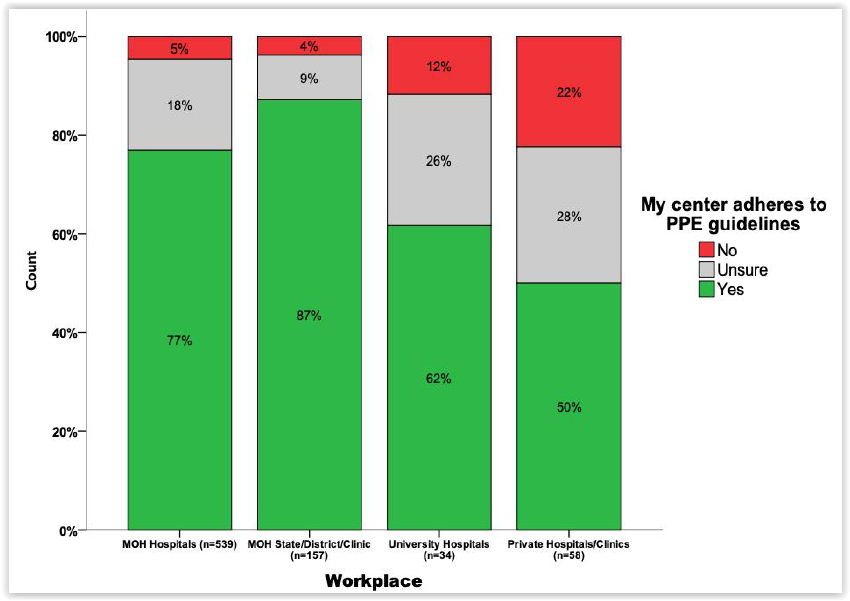
A large majority of health care workers from public facilities said their centre adhered to PPE guidelines at 87 per cent in state health departments, district health offices, and public health clinics; followed by 77 per cent in MOH hospitals; and 62 per cent in university hospitals. Only half of respondents from private clinics and hospitals, however, said their centre followed PPE rules.
MOH hospitals and clinics had the highest percentage of respondents who agreed/strongly agreed that their facility gave sufficient education on PPE guidelines at 74 per cent, followed by university hospitals at 62 per cent. Only slightly more than half, or 54 per cent, of respondents from private clinics and hospitals felt their centre educated staff enough about protective gear guidelines.
“Issues surrounding PPE in Malaysia are the lack of adequate supply; and the need for a more transparent and effective distribution system to and within each health care facility, be it public or privately owned,” survey authors concluded.
“Consensus regarding PPE guidelines and adherence to these protocols must be established and implemented firmly while education strategies regarding PPE usage needs to be improved.”
Survey authors also noted that certain centres, such as some private facilities, were using their own PPE protocol that differed from MOH guidelines.
“Lack of compliance to the guideline will in turn lead to inappropriate use of PPE hence contributing to the shortage of PPE,” they said.
“There are also suggestions given for revision of the PPE guideline to include consideration of the fact that there are high risks encountering ‘probable patients’ at ‘low-risk’ areas, including administrative areas and also departments which do not directly deal with Covid-19 patients, for example orthopaedic surgery, dermatology, ophthalmology and others.
“This is because the chances of encountering probable patients are always there given that asymptomatic transmission is a valid concern.”
The survey authors, who clarified that their poll was conducted informally as a group of Malaysian doctors without affiliation to any organisation, recommended a national stockpiling of PPE coordinated between MOH and local companies, factories, and small and medium enterprises (SMEs) to ensure a steady supply of locally produced protective clothing.
They also called for the creation of a single unit to be in charge of PPE needs assessment and distribution nationwide, noting that such units varied from one centre to another, causing confusion in the standard of protocol and distribution methods.
They further urged for the revamp of the current PPE distribution and request system, saying that adequate supply was not reaching all health centres.
Each health facility should also have a centralised transparent database of PPE stock, which should be able to be accessed by every head of department to ensure check and balance in distribution, besides allowing health care workers using PPE to provide feedback directly to those in charge of needs assessment and distribution.
The doctors also called for a review of PPE guidelines to increase protection for health care workers not working in high-risk areas, like Covid-19 wards or the ICU, as well as to get stakeholders to agree to a common PPE guideline in all health facilities.
“Although the MOH has recently given reassurance that the PPE supplies are adequate; there are many areas that require improvement in order to ensure that Malaysia is well prepared should we have to face another wave of Covid-19 pandemic.”
Authors said their survey was not a proper randomised study, but declared that they did not have any conflicting interests. They also acknowledged their small sample size of 788 respondents, representing about 0.47 per cent of the total health care worker population in Malaysia according to 2011 data.
Most respondents were from MOH hospitals at 539 people; followed by 157 from state or district health departments, public health clinics, and other government institutions; 58 from private clinics and hospitals; and 34 from university hospitals. Doctors comprised 47 per cent of respondents, while the remaining 53 per cent were nursing, allied health care workers, and support staff.
The survey had asked respondents questions in relation to their experiences over the past one month at the height of the Covid-19 pandemic. Malaysia has reported nearly 6,500 confirmed coronavirus cases as of yesterday, while daily infections have been dropping to below 100 since April 17, except for two days on May 2 and 3 that recorded above 100 cases.








