China notified the world on 31 December 2019 of an unusual pneumonia, which is now known as Covid-19, the cause being SARS-CoV-2. It has spread globally with more than 32 million cases and reported its millionth death on 28 September 2020.
It is perhaps an opportune moment to reflect on the pandemic nine months on.
Progress
From zero knowledge at the outset, there has been considerable growth in the understanding about the virus. The progress has been due to the unprecedented global effort by scientists and clinicians.
However, there are still several gaps in the understanding of the disease and the clinical and public health management of the pandemic.
SARS-CoV-2 is not just a respiratory virus as it also affects blood vessels, causing thrombosis and strokes. Although rare, children can be affected with the multisystem inflammatory syndrome, which resembles Kawasaki disease. Covid-19 symptoms can be respiratory, gastrointestinal, cardiovascular, neurological and others. The clinical features of the disease may be dictated by a combination of direct and indirect factors.
The viral genetic code has been cracked with more than 80,000 viral sequences discovered thereby facilitating the tracing of its spread.
The mode of spread may be through direct contact or indirect spread through respiratory droplets. There is also evidence that Covid-19 may spread through aerosols – tiny droplets which can travel farther and could increase the risk of infection in poorly ventilated indoor spaces. Asymptomatic spread has now been acknowledged.
Several drug trials are being undertaken to find treatments e.g. the World Health Organization (“WHO”)’s Solidarity Trial and the United Kingdom (“UK”) Recovery trial.
The Recovery trial reported that the steroid, dexamethasone, reduces the risk of death by a third for patients on ventilators and by a fifth for those on oxygen. Additional data suggested that another steroid, hydrocortisone, is equally effective. Both drugs are cheap, which means it can be used globally.
Remdesivir, an antiviral originally developed to treat Ebola, has been found to reduce the duration of symptoms. However, it has not been shown to save lives, although studies are continuing.
The initial reports on Interferon beta suggests that it reduces the likelihood of hospitalised patients developing severe disease, but larger clinical trials are needed.
The US Food and Drug Administration (“FDA”) has given emergency authorisation for convalescent plasma from those who have survived a Covid-19 infection to treat patients with severe disease. However, some experts are of the view that the jury is still out on its effectiveness. There are separate UK trials on the use of convalescent plasma.
There are also trials on monoclonal antibody cocktail, whose objective is to keep people out of hospital altogether. Preliminary data has been promising. Unfortunately, if the pandemic continues its relentless spread, there would be insufficient supply, if this treatment is found to be effective.
Vaccines would protect against Covid-19 infection, rather than treat it. According to the WHO, there are 169 candidate vaccines at various stages of developments, with nine at the stage of Phase 3 trials. It is expected that some vaccine(s) will be available at end 2020 or early 2021.
Global Data
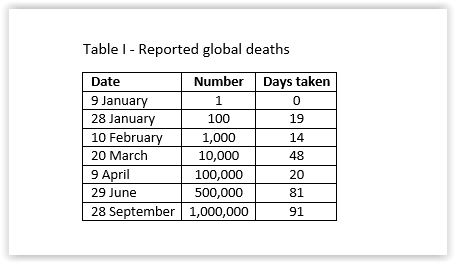
The time it took to reach the tombs globally for the reported Covid-19 deaths are shown in Table I.
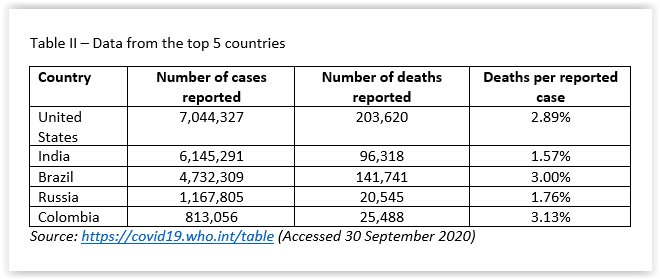
The top five countries with reported Covid-19 cases i.e. the USA, India, Brazil, Russia and Colombia comprised 62% of the cases and 49% of the deaths, with variable deaths per reported case. About 1/5 of the global deaths were reported by the USA. (Table II).
The top five in ASEAN with reported cases were Philippines, Indonesia, Singapore, Myanmar and Malaysia, in descending order. The top five of number of reported deaths were Indonesia, Philippines, Myanmar, Malaysia and Thailand. The top five of reported deaths per reported case were Indonesia, Vietnam, Myanmar, Brunei, and Philippines. No deaths were reported by Cambodia and Laos. Although Singapore reported 57,715 cases, its reported deaths per reported case was 0.05%. (Table III)
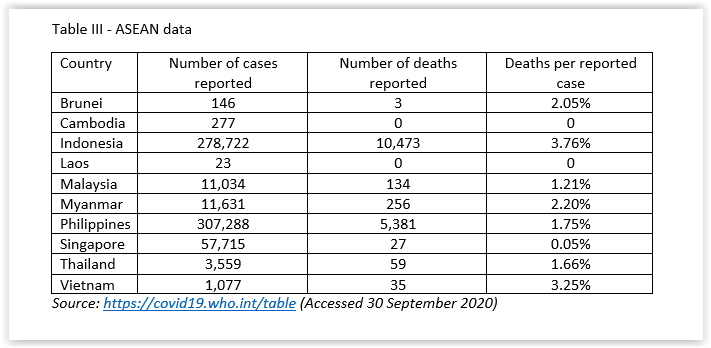
The actual numbers of cases and deaths will not be known. It is thought that there is significant under-reporting of cases and deaths in many countries, either for political reasons, lack of capacity, or even denial.
Some countries report anyone who dies with Covid-19 as a death from the virus even if it is not the direct cause. Deaths at home are less likely to be counted than that in hospitals in many countries, even developed ones.
Mike Ryan, the World Health Organization (“WHO”) emergencies expert, stated: “If anything, the numbers currently reported probably represent an underestimate of those individuals who have either contracted Covid-19 or died as a cause of it…When you count anything, you can’t count it perfectly but I can assure you that the current numbers are likely an underestimate of the true toll of Covid.”
What the numbers tell is that many have been infected and died from Covid-19, and many lives have been cut short.
The assessment of excess mortality data would come much later when the data could be collected and analysed, months and years, after the acute phase of the pandemic have ended. When data about cause-specific deaths are available, the numbers can be unravelled.
A study published in July 2020, “Magnitude, demographics and dynamics of the impact of the first phase of the Covid-19 pandemic on all-cause mortality in 17 industrialised countries“, estimated 202,900 excess deaths in 17 countries between mid-February and the end of May, mostly in England, Wales, Italy and Spain. The confirmed global number over the same period was less than 100,000 deaths.
Although the data on the reported deaths are less than perfect, the picture is that of a pandemic that has escalated at an astounding speed since February 2020 and has yet to slow down.
The impact on the living is no less astounding with economic recessions, lockdowns, increased inequity, adverse impacts on individuals’ physical and mental health and stresses on health care systems. The cracks in the social fabrics of many societies have been laid bare.
Malaysian Data
Whilst the numbers in Malaysia were controlled in the past six months, it has surged in the past 10 days or so (Table IV).
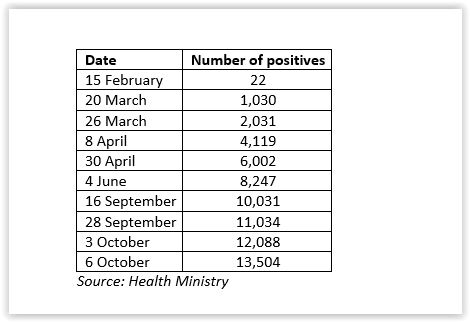
Figure 1 – Daily New Cases
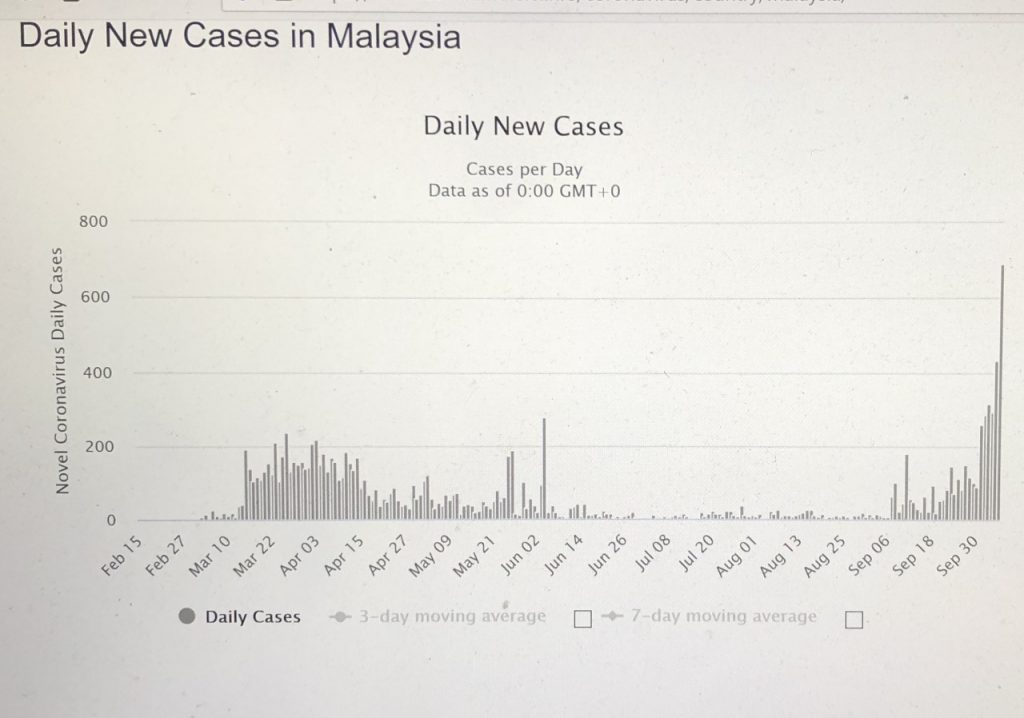
Figure 2 – Active cases
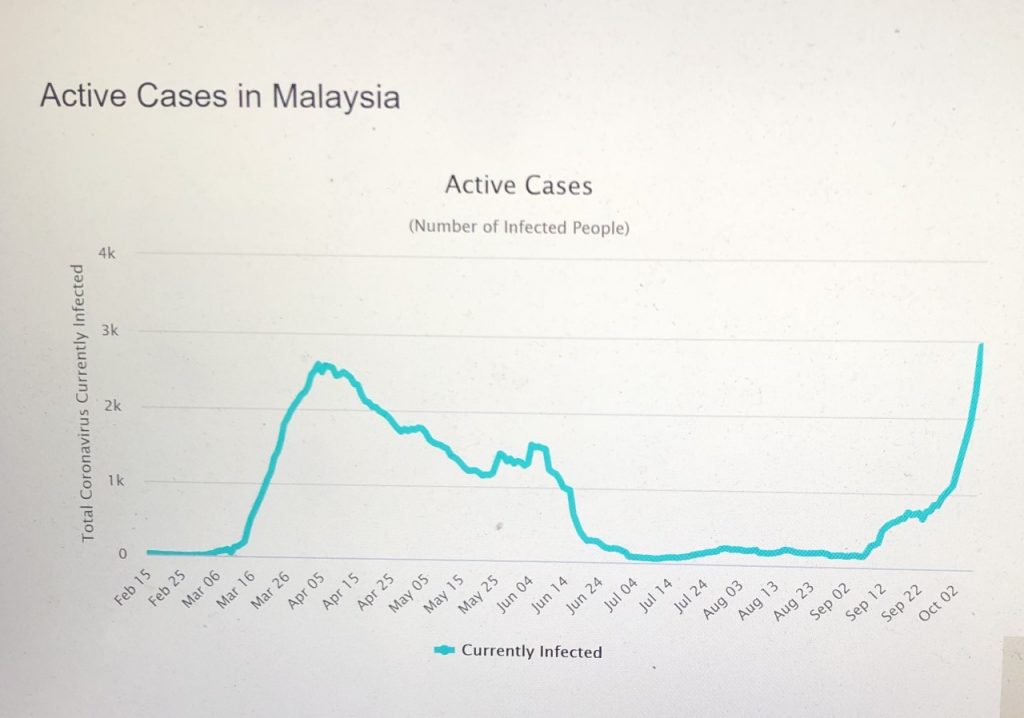
The 2,936 active cases on 6 October has exceeded the 2,596 cases on 5 April. The trajectories of the number of the new and active cases daily is obvious from Figures 1 and 2 above.
What is driving the surge? What does the data show? Have the breaches, exemptions and/ or relaxations of the SOPs contributed to the surge? Frank answers are needed from the Health Ministry.
Whither?
The initial containment was achieved through the tremendous efforts of the public with healthcare staff and other frontline personnel playing pivotal roles.
The Health Minister stated on World Patient Safety Day on 17 September 2020 that more than 600 health care staff had been infected by the virus since February 2020, with 406 in the Health Ministry and the rest in private and university health care facilities. He stated that among the concerns raised by the Health Ministry staff were stress from being away from family, having to comply with strict standard operating procedures (SOPs), exhaustion and issues concerning the Covid-19 special allowance.
In general, the public have complied with the SOPs instituted since the Movement Control Order (“MCO”) came into force on 18 March 2020. There were unsubstantiated claims that complacency and fatigue have set in after more than 200 days of the MCO.
The public are constantly reminded by the authorities to comply with the SOPs. The punishments for non-compliance have varied from fines to imprisonment. However, some of the punishments have been disproportionate. Some were fined and some jailed for varying terms.
There is an impression that there are differing standards in the enforcement and punishment for non-compliance with SOPs – even between a Minister and Deputy Minister.
It is difficult to fathom how some individuals, particularly those in positions of authority, consider themselves invincible against the SARS-CoV-2 virus. Instead of setting an example for the public, some of those in authority, who are remunerated by taxpayers, have disregarded the SOPs.
Some of the policy decisions were peculiar, to say the least.
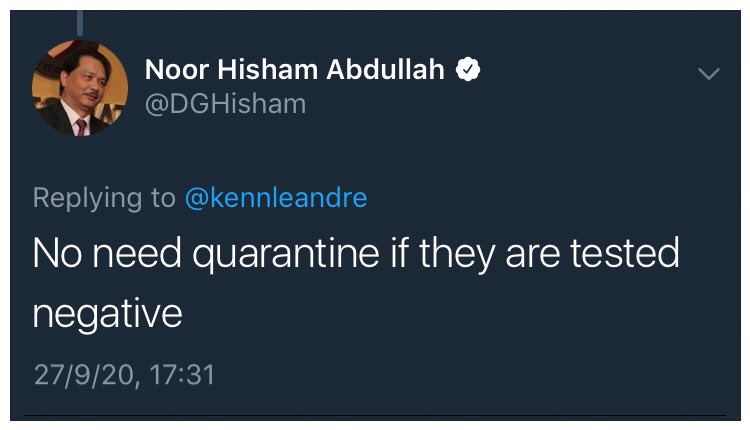
For example, when there were increasing numbers of positive cases in Sabah in early to mid-September, there was no requirement for testing and home quarantine for those who had been to the red zones in Sabah. The Health Ministry’s statement that there was no need for home quarantine when the first test was negative was bizarre. Was the statement based on science?
Some have attributed the recent surge to the failure to physically distance, use masks and home quarantine. There is validity to this position as the media images of the campaigning in the Sabah elections illustrated the adage that a picture is worth a thousand words.
Similarly, the government announced, on 6 October, a travel ban on interstate travel to and from Sabah from 12 to 25 October. Is the virus going to wait till the ban comes into effect? Will the travel ban affect travel to and from non-red zones in Sabah, which has an area of Pahang, Terengganu, Kelantan and Kedah combined?
What was the position of the health professionals in the Health Ministry in both decisions? Were they involved in the decision making? Was health the primary consideration in the decisions?
The public and medical professionals have called for compliance with the SOPs by everyone, irrespective of their position in society. There should be equal treatment, in accordance with the law whoever, whenever and wherever the SOPs are breached. There cannot be one rule for the common man and another for the privileged gentry.
The Prime Minister has assured that everyone will be treated the same and that the rotan may have to come out. Only time will tell whether there is a gap between reality and rhetoric.
Apologies have little or no value when others have been exposed to infection through irresponsible behaviour.
In an interview with Bernama reported on 22 September 2020, the WHO representative to Malaysia, Singapore and Brunei stated that she thought Malaysia was prepared to handle an increase in Covid-19 cases, but several weaknesses had to be addressed. These included preventing infections in closed and confined settings like detention centres, prisons, and improvements in the surveillance system with the participation of the private sector.
Compliance with standard operating procedures (“SOPs”) have to be monitored. Expanded testing would facilitate testing and searching for cases, which is an important strategy to prevent further spread.
Choice is not an option. The authorities have to apply the law and SOPs equally if the public is expected to comply.
Technology has yet to be utilised to its capacity. What is needed is to utilise real-time data and artificial intelligence in enhancing epidemiological capabilities to target, test, contact trace and isolate.
Rest assured, the virus does not discriminate on gender, ethnic origin, religion, position in society and time.
In summary, public trust, the pillars of which are transparency, accountability and fairness, is critical if the spread of Covid-19 is to be contained. Failure to obtain public trust will lead to a quagmire that will be very difficult to extricate from.

Dr Milton Lum is a past President of the Federation of Private Medical Practitioners Associations, Malaysia and the Malaysian Medical Association. This article is not intended to replace, dictate or define evaluation by a qualified doctor. The views expressed do not represent that of any organization the writer is associated with.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.








