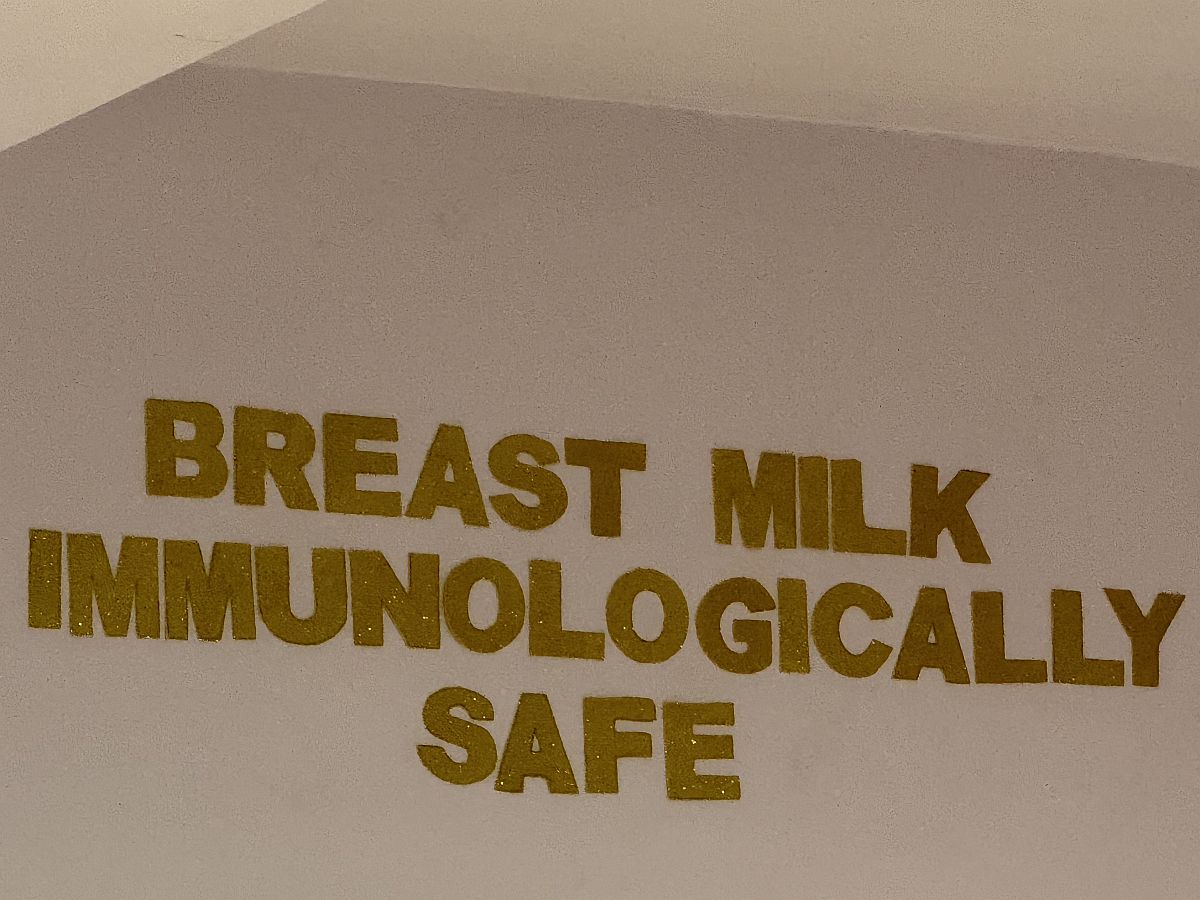
During a recent visit to a leading maternal and child health hospital in Kuala Lumpur, a public-facing statement displayed along the arch of a walkway corridor described breast milk as “immunologically safe”.
The phrase is misleading; risks reinforcing harmful assumptions and warrants critical review to ensure accuracy and clarity in public health messaging.
Since breastfeeding is the earliest and most foundational public health intervention, ensuring its protection is critical to safeguarding population health from the very beginning of life.
While likely intended to reassure, the phrase worrisomely understates the biological, psychological and social reality of breastfeeding as a holistic and interconnected act between mothers, infants, and their broader social, cultural, institutionalised, and political environment.
Such safety-orientated messages about breast milk’s immunity undermines maternal confidence by shifting focus from embodied knowledge to biomedical validation.
This fosters anxiety, reliance on measurements and doubt–hence reducing breastfeeding from a dynamic, life-sustaining process to a medical product.
The Problem With ‘Safe‘
To call breast milk merely “immunologically safe” is to misrepresent its true nature.
Breast milk is dynamically bio-adaptive and evolutionarily irreplaceable. It changes in real time in response to infant illness, maternal health, and environmental stressors.
It contains immunoglobulins, microbiota, stem cells, oligosaccharides, hormones and anti-inflammatory agents that support neurological development, regulate infant physiology, and build lifelong immunity for infants, while also offering a surplus of health benefits for mothers, including reduced risks of certain cancers and improved postpartum recovery.
These are inimitable and cannot be replicated by any artificial substitute or infant formula. Therefore, labelling breast milk as solely “safe” within health systems conceals the truth about its complex bioactive properties and risks equating it with formula milk–opening the door for infant formula companies to exploit this ambiguity and market their products as equivalent or technologically superior.
Moreover, when institutions substitute the word ‘breastfeeding’ with “breast milk”, they disembody a profoundly relational and responsive act.
Breastfeeding is not simply the transfer of milk; it is a symbiotic interaction between mother and child–shaped by mutual responsiveness and attachment.
Describing breast milk without breastfeeding reduces mothers to objects of reproduction–rather that active agents of caregiving and health. This supresses the adaptive co-agency of the maternal-infant dyad.
Amid rising economic precarity and climate-related disruptions, Malaysia continues to see low exclusive breastfeeding rates in underprivileged populations.
While the causes are complex and multifactorial (work, lack of knowledge, misconceptions about breastfeeding, lack of support from families and communities, medical conditions), this context underscores the need for public messaging that affirms breastfeeding as essential health.
Malaysia’s Opportunity And Responsibility
Malaysia has made commendable progress through the Baby-Friendly Hospital Initiative (BFHI) and national nutrition policies. Yet underserved populations, including Orang Asli, urban poor (B40), forced migrants, and stateless persons, continue to face systemic barriers to breastfeeding support.
In remote, informal, or flood-affected settings where clean water and refrigeration are lacking, breastfeeding provides critical and sustainable nourishment, protects from waterborne diseases and reduces infant mortality, serving a vital first-line form of defence.
This calls Malaysia to not only invest in human resources and programmes, but also scrutinise the language that shapes public understanding and policy discourse.
Placing Mothers At The Heart Of Public Health
This year’s World Breastfeeding theme, “Prioritize Breastfeeding: Create Sustainable Support Systems”, under the World Health Organization’s (WHO) Healthy Beginnings, Hopeful Futures campaign for 2025, will focus on supporting women and babies need from the healthcare system through their breastfeeding journey.
Given that reductionism risks fragmenting the scientific, economic and social significance of breastfeeding, this article calls for health messages that reflect both evidence and dignity, such as:
- Breastfeeding is Superior Nutrition: Made by Your Body, Attuned to Your Baby’s Needs
- Penyusuan Susu ibu Adalah Pemakanan Terbaik: Dihasilkan oleh Tubuh Anda, Peka terhadap Keperluan Bayi Anda
This shift in language affirms the biological and relational significance of breastfeeding, recognises optimal nutrition for vulnerable infants, and validates confidence in the maternal body’s natural design for motherhood and nurturing.
Recommendations for Malaysia’s Systems
To prioritise breastfeeding as essential for child health and survival, governments must undertake unified whole-of-system actions across ministries, public-private partnerships, and civil society sectors:
- Audit and revise all public-facing materials to reflect accurate and empowering language.
- Strengthening enforcement of the International Code to ensure health communications are not shaped by commercial interests.
- Tailor inclusive, multilingual materials and breastfeeding education according to health literacy levels of underserved populations.
- Invest and scale up culturally responsive lactation training across health facilities, networks, and NGOs.
- Integrate grassroot-led breastfeeding support systems across antenatal, postpartum care, KOSPEN programmes, and early childhood development outreach programmes.
- Facilitate cross-sector collaboration between key ministries to support enabling breastfeeding environments.
- Family-friendly workplaces and community policies, especially in informal labour.
Conclusions
Language used to describe breastfeeding shapes public consciousness, informs policy, and either honours or obscures the biological and emotional power of the maternal-infant bond.
Grounded in the principles of health justice and human dignity, this article calls on Malaysia’s policy machinery, communities and institutions to strengthen governance through clear decision-making structures and better coordination.
Only through precise, respectful language can systems support breastfeeding, empower mothers and protect children.
June Joseph is a medical anthropologist specialising in breastfeeding, maternal and child health and nutrition, health equity, systems accountability, and good governance. She is an Honorary Senior Fellow with the University of Queensland, Australia.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.