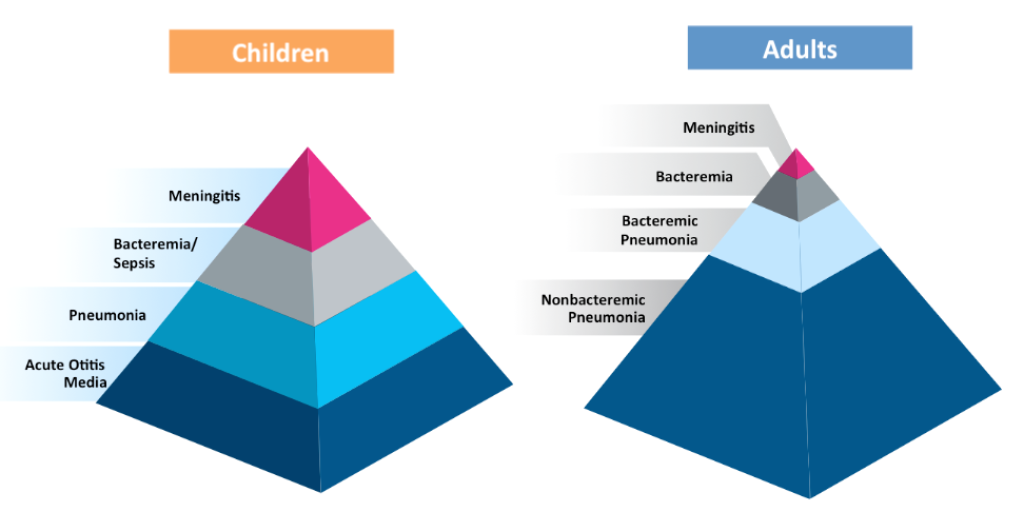
Pneumococcal disease (PD) presents itself differently in adults compared to children. In adults, pneumococcal pneumonia constitutes the vast majority of disease. In young children, acute otitis media is by far the most common presentation of PD.
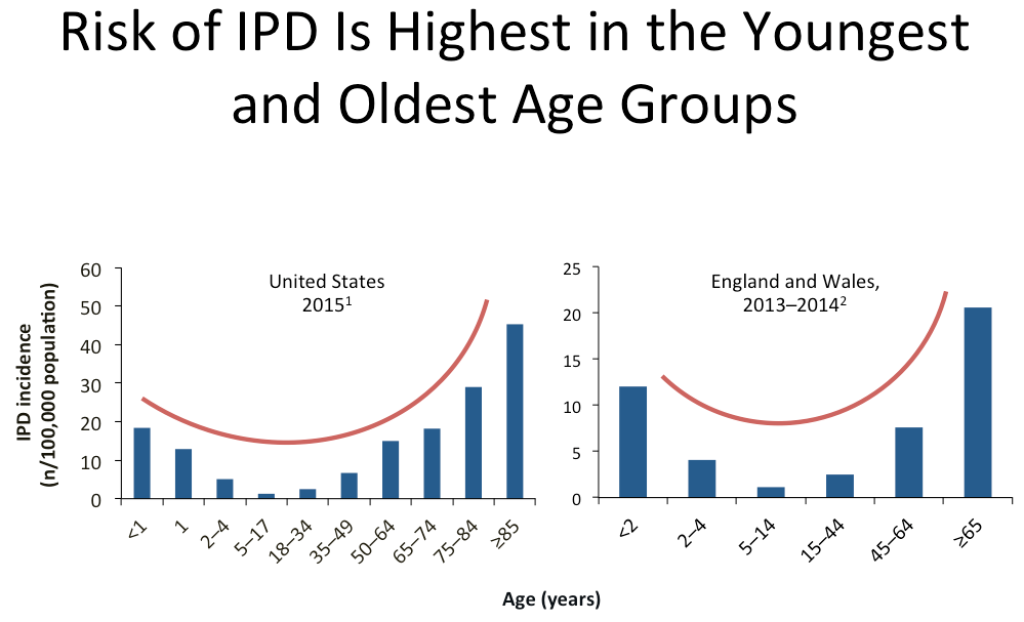
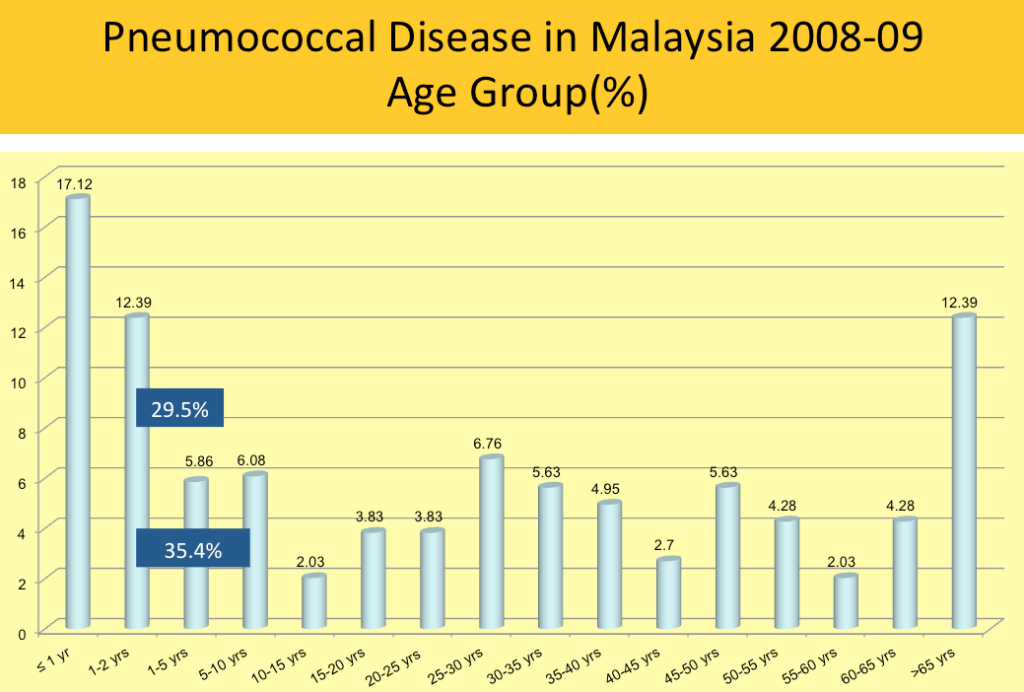
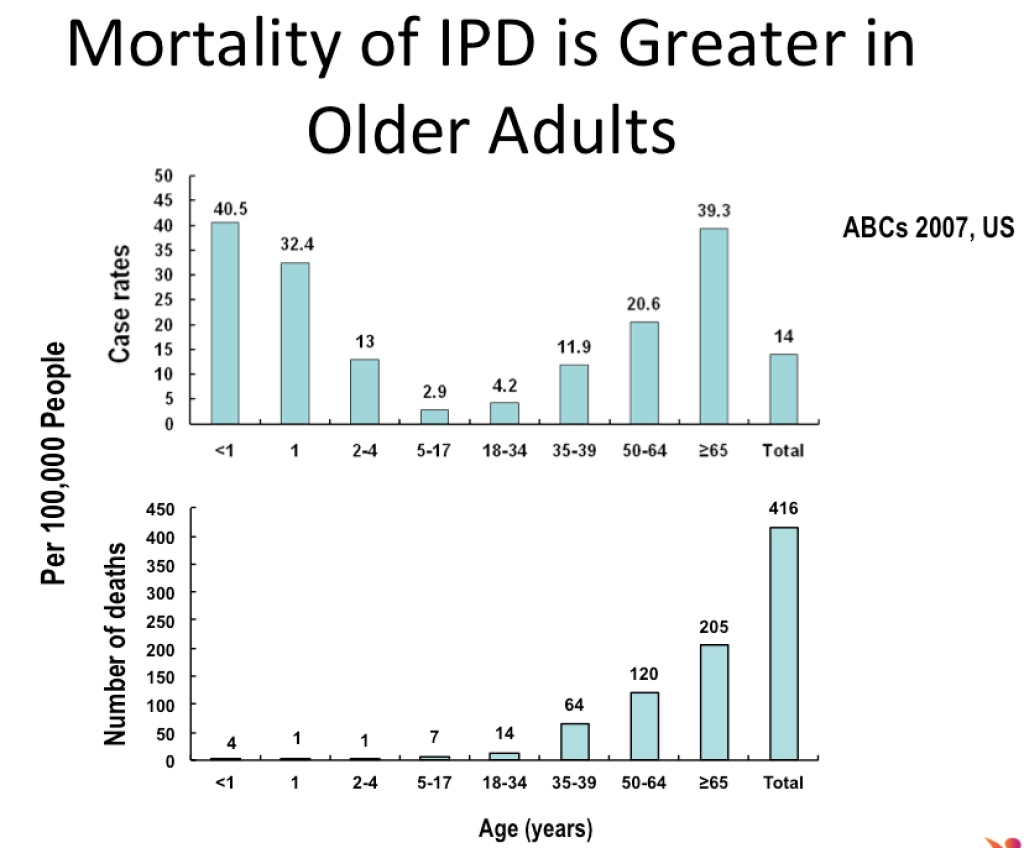
Epidemiological surveillance shows that the youngest and oldest age groups have the highest incidence of invasive pneumococcal disease (IPD).
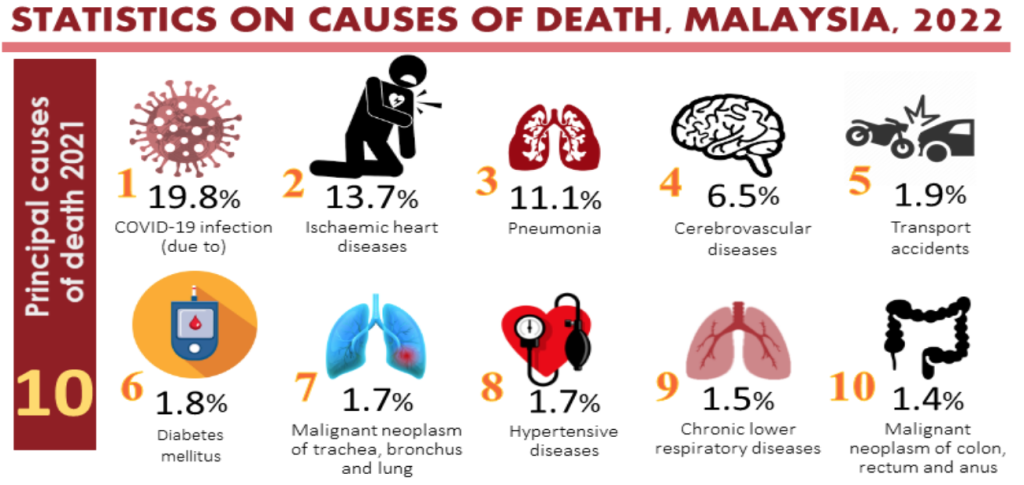
In 2021, pneumonia was the third most common cause of death in Malaysia. The common causes of pneumonia include Streptococcus pneumoniae, influenza, and recently, SARS-CoV.
Using modern techniques including polymerase chain reaction (PCR), the aetiology of community acquired pneumonia (CAP) can be determined more accurately, with Streptococcus pneumoniae contributing 38 per cent and respiratory viruses 29 per cent. Streptococcus pneumonia is the most common bacterial pathogen for CAP and hospital acquired pneumonia (HAP).
Many adult patients, 50 years and older, reported experiencing a worsening of their pre-existing health conditions, following a diagnosis of CAP.
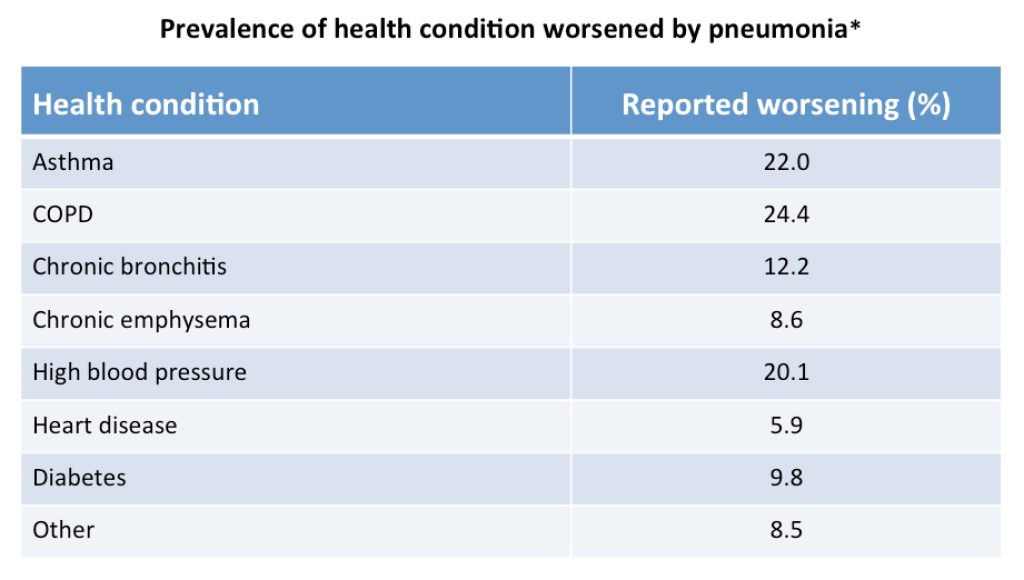
Chronic Obstructive Pulmonary Disease (COPD) patients with CAP are nine times more likely to be hospitalised. Adults hospitalised with pneumococcal pneumonia are at increased risk of major cardiac events, resulting in a significantly increased risk of mortality. Mortality of IPD is higher in older adults, especially those more than 65 years old.
Two vaccines are currently available for the prevention of IPD in adults. These are the pneumococcal polysaccharide vaccine (PPV) and the pneumococcal conjugate vaccine (PCV).
The benefits of the PCV over the PPV is as illustrated in the table below.
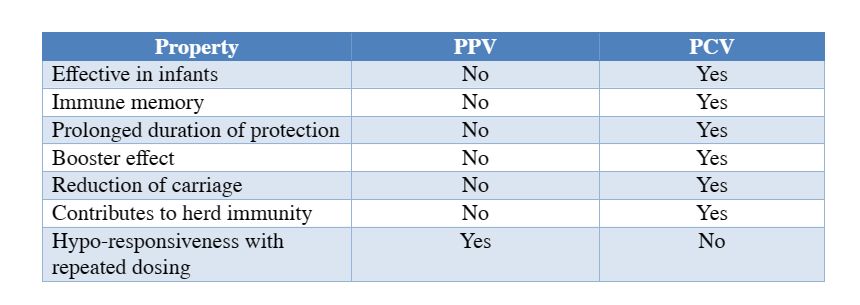
The following statement from the World Health Organization (WHO) sums up the issues with the PPV: “Despite multiple studies conducted during more than 30 years, the efficacy and effectiveness of PPV23 (23 valent) in children and adults remain poorly defined and the subject of the controversy”.
The safety and efficacy of the PCV13 (13 valent) was demonstrated in the Community Acquired Pneumonia Immunization Trial in Adults (CAPiTA).
PCV13 demonstrated a vaccine efficacy (VE) of approximately 46 per cent against a first episode of any vaccine-type (VT) pneumococcal CAP.
PCV13 convers greater protection against a first episode of VT-IPD, with a vaccine efficacy of 75 per cent.
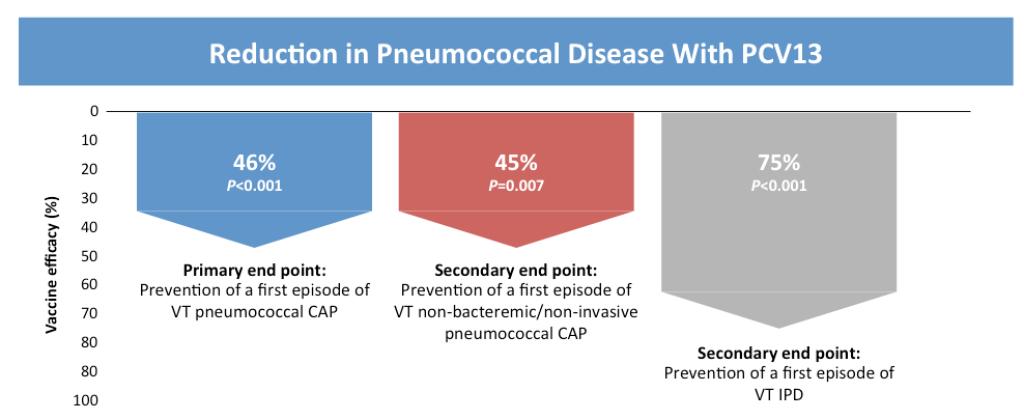
Post-hoc analysis showed that the PCV13 efficacy continued to remain persistent against vaccine-type CAP and IPD throughout the duration of the study (4 years).
In a real-world setting study, PCV13 reduced the risk for hospitalised VT-CAP by 73 per cent in adults aged 65 and older, including those with comorbidities. This reinforced the PCV13 vaccine efficacy observed in CAPiTA.
The current influenza outbreak is often complicated by secondary bacterial infections (35 per cent). and S pneumoniae has been shown be a frequent cause of influenza-related bacterial pneumonia.
CAP (including pneumococcal pneumonia) in adults, especially in the presence of pre-existing comorbidities is associated with significant utilisation of health care resources, which contributes to a substantial burden on health care systems.
PCV13 in adults has been shown to be efficacious against vaccine-type CAP and IPD and can help to offset the strain on finite health care resources.
Adults with pre-existing comorbidities associated with increased risk of IPD, persons above 60 years and persons attending mass gatherings (e.g. Hajj) are recommended to take a single dose of PCV13.
Newer generations of PCV, namely PCV15 and PCV20 (currently not available in Malaysia), promise to further widen the coverage of pneumococcal serotypes and claim better efficacy against certain serotypes.
Dr Musa Mohd Nordin and Dr Husna Musa are paediatricians.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.





