SUBANG JAYA, August 4 — Countries in Southeast Asia are among the few globally with an increase in youth smoking over the past three decades, unlike Europe and the United States that permit the use of e-cigarettes, a professor claimed.
Lion Shahab, a professor of health psychology at the University College London (UCL) – whose current research focuses on novel smoking cessation interventions amongst other tobacco-related research – touted e-cigarettes as a suitable harm reduction method to cut smoking rates.
“The good news is that across the world, people have reduced their per capita cigarette consumption. People smoke fewer cigarettes. But if you look at the number of smokers, people who are individually affected, only countries or parts of the world that have primarily embraced e-cigarettes has there been a decrease over this time period from 1990 to 2020.
“I’m not saying e-cigarettes are the only reason for this, but it is the case that in Europe and in America, there’s a reduction in the number of smokers. And if you are concerned about youth effects, youth trends, I’m afraid to say Southeast Asia is one of the few countries where you can see an increase in the use of youth smoking over the last 20 or so years.
“There’s been a decrease everywhere else. It remains a problem, particularly in Southeast Asia. And e-cigarettes have the potential to be a game changer, I believe. They’re relatively cheap. People are essentially self-funding this, whereas treatments such as Varenicline or NRT (nicotine replacement therapy) is quite expensive, and people have to pay for that themselves,” Shahab said at a forum on e-cigarettes held at Monash University Malaysia last July 12.
According to the Tobacco Atlas’s regional trends in smoking prevalence of young teens, which was cited by Shahab, there was a 1.4 percentage point increase in the number of teen smokers aged 13 to 15, from 8.8 per cent in 2000 to 10.2 per cent in 2010 for the Southeast Asia region.
Despite the above findings on region, Malaysia’s recent National Health and Morbidity Survey (NHMS) 2022 painted a very different picture from the 2010 Tobacco Atlas data.
Malaysia experienced a 7.6 percentage point drop in teenage smokers aged 13 to 17 years from 13.8 per cent in 2017 to 6.2 per cent in 2022. However, this decline was accompanied by a rise in the use of e-cigarettes among adolescents, from 9.8 per cent in 2017 to 14.9 per cent in 2022.
The simultaneous fall in smoking and rise in vaping suggests that Malaysian adolescents may be swapping cigarettes for vape.
Despite Shahab’s claims about reduced harm from e-cigarettes, the Malaysian context is very different from other countries that regulate vape that impose limits of 2 per cent nicotine content. Currently, e-cigarettes and vape with nicotine can be sold legally to anyone in Malaysia, including minors aged below 18, after the government declassified liquid nicotine as a scheduled poison last March 31.
The Problem With Data On Harm From E-Cigarettes
The data surrounding the harm resulting from e-cigarettes, according to Shahab, is hard to interpret.
The main reason for this is that most e-cigarette users are former smokers, making it difficult for researchers to ascertain whether the harm comes from the use of e-cigarettes or from the long-lasting effects of the cigarettes smoked prior to transitioning.
To illustrate the above point, Shahab drew from the British Doctors Study to demonstrate how some of the effects on health that result from smoking cigarettes are irreversible.
The study, which began in 1951, was the world’s first and largest prospective study of the effects of smoking to establish a convincing link between tobacco smoking and cause-specific mortality.
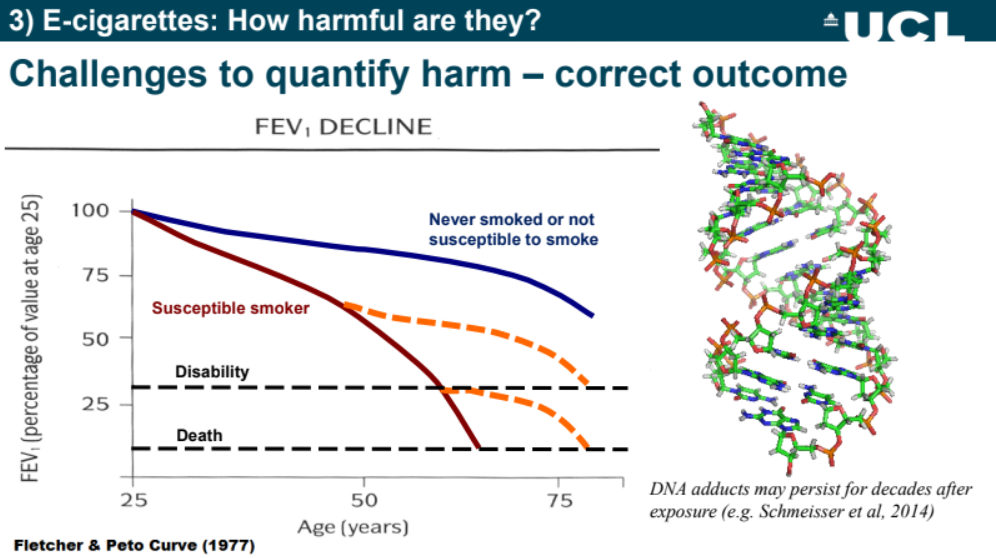
The graph provided by Shahab depicting the Fletcher-Peto Curve diagram shows how smoking can result in disability and death, and how even after a person stops smoking, they are still more likely to die later on as a result of their exposure to cigarettes.
“Some of these related health effects are therefore irreversible. So if we wanted to look at health outcomes in the population, we don’t have enough data at the moment to do this really because there haven’t been around enough e-cigarettes.
“And then if you looked at that population, because most of them have been past smokers, if you see any effects, they might be confused with their previous smoking behaviour. So I don’t think it’s a good thing to look at our health outcomes at the moment,” said Shahab.
Because of the above, Shahab said the best way to assess harm reduction is by observing the biomarkers of risk or exposure.
When a person comes into direct contact with a chemical, a substance corresponding to the chemical may be found in the body, and this is called a biomarker of exposure. These biomarkers of exposure are often the products of metabolism and can be measured in the urine, blood, saliva and hair. The level of a specific biomarker in the body measures the extent to which a person may be exposed to a chemical.
Shahab’s support for this method of measuring harm is that the evidence for this biomarker accumulates quickly. They are short-term markers, and thus, avoid the overlap between the health outcomes that could stem from past cigarette smoke and the health outcomes related to e-cigarettes.
With that being said, Shahab warns people not to overemphasise animal research that uses these biomarkers, as it does not reflect the reality of how e-cigarette products are used.
Citing a 2019 study by Proceedings of the National Academy of Sciences of the United States of America (PNAS) titled “Electronic-cigarette smoke induces lung adenocarcinoma and bladder urothelial hyperplasia in mice”, Shahab held that the suggestion made by the study of how e-cigarettes cause lung cancer is problematic as the researchers in this study used a mouse breed that spontaneously develops cancer within the year, and the exposure that the mice were subjected to did not translate into real-world exposure.
“Then these poor mice were exposed for four hours or five days a week at an exposure of 36 milligrams per millilitre. That’s a huge amount of exposure. It’s basically like vaping seven years worth of e-cigarettes in one year. It was so aversive that three mice just died due to non-cancer causes. These mice are stuck in a cage filled with aerosol.
“If you use a device [with] a constant voltage for four hours, it leads to overheating, and then you create carbonyls, which are themselves harmful. The other thing that happens is if you smoke or vape, your body has homeostatic responses: you stop, you start, you stop.
“That’s not the case if you essentially put it into what is essentially a gas chamber.
“The other thing is that you have additional exposure, because nicotine deposits both on the fur, and mice lick their fur, as well as on the surfaces. And if you leave nicotine exposed, it can oxidise to NNK (nicotine-derived nitrosamine ketone), which is a tobacco-specific nitrosamine which is highly carcinogenic. This study finds it causes cancer.
“But in fact, there’s very little evidence that nicotine causes cancer. In IARC (International Agency for Research on Cancer), the international research consortium run by the World Health Organization (WHO) also confirms that nicotine doesn’t cause cancer at this stage anyway, as far as we know. So I think it’s important not to overstate animal research because of these problems of translating it to humans.”
IARC states that nicotine does not cause cancer directly and its effect is to make tobacco addictive, and people who are addicted to nicotine are more likely to continue to expose themselves to carcinogens in smoked or smokeless tobacco.
While animal studies have their problems, the same also can be said for human studies. Referring to a Portland State University study – which found that e-cigarettes produced formaldehyde levels that were far higher than conventional cigarettes when the volt settings on vape devices were set at the highest level – Shahab said regular e-cigarette users would not be overheating their devices, and there would be no risk of being exposed to the levels of formaldehyde discovered in the study.
“Of course, if you overheat the e-cigarette, you would create harmful substances, such as formaldehyde.
“It’s very, very unpleasant. It’s called dry puff. And no vaper who uses the product would continue because it’s very acrid, very unpleasant. You stop it immediately. So people wouldn’t realistically be exposed to these kinds of levels because they wouldn’t overheat their e-cigarettes. So one of the reasons why I think it’s better to look at body level exposure is because we know then we control for the user interaction with the device.”
NNAL Good Yardstick For Measuring Harm
Shahab argued that the first and best biomarker is NNAL, a product formed after 4-(methylnitrosamino)-1-(3-pyridyl)-1-butanone (NNK) enters the body. NNK belongs to a group of chemicals called tobacco-specific n-nitrosamines (TSNA), and this group of chemicals is found only in tobacco products.
Measuring NNAL in people’s urine is a reliable way to determine exposure to NNK for smokers, for non-smokers exposed to environmental tobacco smoke (ETS), and for people who use smokeless tobacco products (chewing tobacco, snuff).
Referring to various studies conducted on second and third-generation e-cigarettes, Shahab, via the use of a bar chart, showed how the level of exposure to this carcinogen decreased over time for smokers who switched to e-cigarettes.
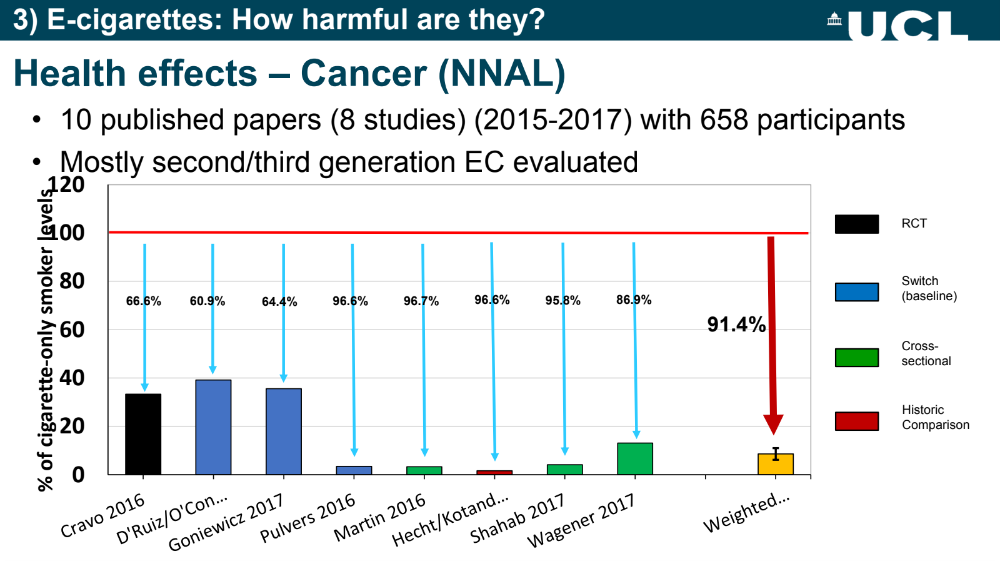
“Here you see the exposure of users of e-cigarettes to this particular carcinogen, which we know causes cancer, compared with people who were smokers. And it’s set at 100 per cent for smokers to see how much more or less exposure there is among people who use e-cigarettes long term. And in terms of long-term, some of these people had been using e-cigarettes from left to right for only a week since stopping smoking, to several years on the right-hand side.
“So as you go from left to right, you will see there’s a change.”
In addition to the above studies, Shahab also asserted that people who use e-cigarettes experience similar chances of getting cancer and other cardiovascular and respiratory diseases as non-smokers, giving credence that e-cigarettes are indeed a harm-reduction product.

The most striking difference between cigarette smokers and e-cigarette smokers can be seen when one looks at the data surrounding dual usage. In the graph shared by Shahab, data for harm across four types of users: dual use (daily smoker/ non-daily e-cigarette user), e-cigarette user only, dual use (daily e-cigarette user/non-daily smoker) and non-users were placed next to each for ease of comparison.
The graph showed the level of exposure and harm these four groups of people face across two cancer biomarkers, brain/ heart/ kidney diseases, and respiratory diseases.
Across each category, the harm e-cigarette users experienced was only marginally higher than people who never smoked.
“So what you can learn from this is, I think that dual use is only beneficial if you’re a non-daily smoker. There’s less impact of e-cigarettes on metals in terms of exposure. And there’s a residual increase in some biomarkers compared to non-smokers. So, obviously reduced risk, but not no risk.”
The above data in addition to other data led Shahab to consider e-cigarettes more akin to nicotine replacement therapy than cigarettes.
“I would put e-cigarettes much closer to nicotine replacement therapy than I would put it to cigarettes, based on the data so far.”








