When the Covid-19 pandemic hit in 2020, many nations realised that they were ill-equipped to deal with the emergence of this novel infectious disease.
This was forecasted in the 2019 Global Health Security report, which reported that no country was fully prepared for a catastrophic biological event, and that up to a third of countries were unprepared.
Public health experts further recognised that early recognition of novel infectious diseases and a rapid response were vital to preserve the health and economy of a population, as well as safeguard the global movement of people and goods.1
Though Covid-19 was recognised in December of 2019 by the World Health Organization (WHO), it was said that the existence of this virus could have started as early as November 2019 in China (or maybe even before that).2 Could this have been a different variant from the Alpha strain?
We might never know, as there were no proper mechanisms in place in many countries that could have been better prepared for a respiratory-linked pandemic.
Despite their best efforts to contain the spread of infection during these unprecedented times, most countries observed several waves of the pandemic over the past two years, with each wave often bringing about more cases and deaths than the one before.
Even though vaccinations have played a major role in reducing the morbidity and mortality due to Covid-19, non-pharmaceutical public health safety measures remain an important government response to curb the rate of infection.3
Some countries imposed permanent guidelines for their citizens to ensure that the pandemic remain under control, which may have led to great disruptions to the economy and individual liberties.
On the other hand, some countries implemented a system of rules, often dubbed the traffic light system, where the “red light” corresponded with highest risk, therefore requiring the highest stringency.4
The level of stringency was typically determined by a set of indicators, such as the burden of disease, test positivity ratios, and vaccination rates and other indicators deemed important by individual countries.5
In Malaysia, the government opted for a response that was based on current needs and conditions. Though nationwide lockdowns were deemed effective and successful at the start of the pandemic, it came at a high economic cost.
Consequently, the priority was to strike a balance between managing the pandemic while maintaining a balance of lives and livelihoods.
Whilst there is insufficient evidence to say which strategy is the best way to mitigate a pandemic of this scale, early intervention was found to be the key in reducing Covid-19 infection and death rates.3,6
Presented here is an overview of the situation in Malaysia, using data accessed from the Covid-19 open-source data repository in the country. At the start of the pandemic, Malaysia observed between 0 to 300 new cases of Covid-19 infection per day (Figure 1).
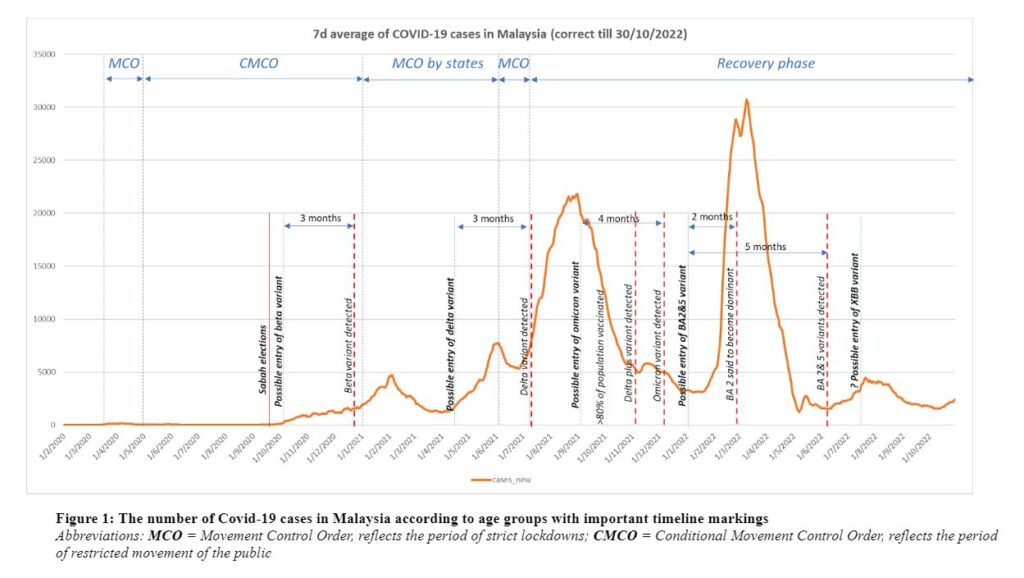
The government imposed strict lockdowns and restricted movement among the public amid rising cases. Malaysia witnessed 7,095 cases and 115 deaths during the first six months of 2020. As observed in Figure 1, the surge in cases in Malaysia correlates to the emergence of new variants of the Covid-19 virus.
However, the detection of these variants was often delayed, by up to 3 months. For example, the United Kingdom (UK) had reported a newer variant was causing a mass surge in cases in October 2020. By the time the Beta variant was reported and made public in the UK, there had already been a significant spread across Europe.7
In Malaysia, we saw an early rise of cases in the middle of September 2020. At the time, many attributed this to local parliamentary elections in an East Malaysian state (Sabah), but the severity of the spread may have been exacerbated by the more infectious Beta variant. The presence of the Beta variant in Malaysia was only detected in December 2020, three months after the peak of the surge.
The next surge in cases was observed between April and August 2021. Corresponding to that, the Delta variant was detected three months after the initial rise in cases. It is also possible that some of the cases during this time was a surge due to the Omicron variant, which was first isolated in Malaysia in December 2021 (again about three months later).
In January 2022, we saw another surge in cases that, likely due to the emergence of newer variants such as the Delta-Omicron or BA.2 or BA.5 variant. However, it was only about five months later that the variant was isolated here in Malaysia.
The current wave might be strongly due to the XBB variant. It is also something to note that the replacement of one dominant variant with another causes the rise of cases.
Without intervention, the surge in cases is expected to rival the previous wave, albeit with considerably lesser deaths in response to high vaccination rates in the country.
The delay in response to emerging virus variants can be attributed to two factors. Firstly, while there has been substantial effort to improve capacity for genomic sequencing in response to the pandemic, it remains insufficient in many countries, especially among lower income countries – due to technology skill, requirements and the costs that revolves around it.
The need to increase the capacity for all countries to conduct efficient genomic sequencing for at least 3 per cent of all confirmed cases, with transparent reporting mechanisms, have been highlighted by the WHO as a key gap in ensuring global pandemic preparedness.
Secondly, non-pharmaceutical public health safety measures are often deployed in reaction to high rates of infection, which may be well too late. It has been shown that early implementation of these interventions is critical to curb the spread of the virus, thereby reducing the number of infections and deaths.3
The delay in response is most likely due to difficulty in recognising an early surge of infections via conventional methods for tracking and monitoring of data, which are often siloed and subject to human capacity and error.
It leads to an imperative lesson – to have the right tools at the right moment that will enable informed and effective data-driven decision-making.
This is, therefore, an area where big data and machine learning can play a game-changing role. Convincingly, a robust pandemic surveillance system built on live data might offer an opportunity for governments to react substantially earlier.
These systems, such as the locally made International Pandemic Preparedness Centre (IPPC) platform developed by AINQA Health, leverage big data and Artificial Intelligence (AI) to ease the management of infectious disease outbreaks.
With effective predictive analytics and modelling, a smart system may be sufficiently sensitive to detect possible uptick in cases, thereby allowing authorities to intervene before the actual spread.
For example, in the context of Malaysia, had action been taken during the initial rise in cases between April and June 2021, we may have observed a significantly flatter curve in the months that followed.
Furthermore, such systems are aligned to current national and international priorities. For example, integrated electronic tools are prioritised in building resilient surveillance systems in the recent WHO benchmarks for the International Health Regulations Capacities. Big data and AI are already being used in China, Taiwan, the United States, Singapore, and India to track the spread of Covid-19 nationally.8
The one positive outcome of the pandemic was the realization that data-driven evidence is critical for timely and effective decision making at national and international levels.9,10
The best way to implement this would be to have a more user-friendly approach for data entry for those keying in data, and allow live time updates on screens of the surveillance rooms — coupled with ongoing information received about potential new outbreaks or clusters.
Having all this information within a system and having alert/action points within this system, will allow the health authorities to alert Malaysians about the rising number and be even consider that perhaps the country has been hit by a more infectious variant.
This will enable us to take the necessary preventive steps especially if the country was to implement the traffic light system for mitigation so that an early proper grasps and control of the situation is possible.
Most countries cannot afford another strict lockdown and closure of borders. Preparedness, therefore, is the best way to prevent another major health crisis and economic disruption.
By continuing to track and monitor infectious disease outbreaks, we can stay one step ahead of the next epidemic or pandemic.
An AI-driven infectious disease surveillance system may offer a cost-effective solution to do so. It allows countries to invest in a health care system that can prevent infectious disease outbreaks, reduce the loss of lives, and preserve the economy in the face of public health threats.
Declaration of interest: Author(s) declared no competing interest.
Acknowledgement: I would like to thank the Ministry of Health Malaysia for making the data on Malaysian Covid-19 deaths publicly available through Github. Also, the author received no specific funding for this work. I would like to thank the following individuals for their input and support towards this article: Nadia Rajaram, Nur Asheila Abdul Taib, Dhesi Baha Raja, Jinat Ahmed, Lidwina Edwin Amir, Quek Yee Theng, and Michelle Chan Yoon Kim.
References
- Haug N, Geyrhofer L, Londei A, et al. Ranking the effectiveness of worldwide Covid-19 government interventions. Nature Human Behaviour. 2020/12/01 2020;4(12):1303-1312. doi:10.1038/s41562-020-01009-0
- LaFee S. Novel Coronavirus Circulated Undetected Months before First Covid-19 Cases in Wuhan, China. Review Article. UC San Diego Health; 2021. March 18, 2021. 25/4, 2022. Accessed 25th of April 2022.
- Hale T, Angrist N, Hale AJ, et al. Government responses and Covid-19 deaths: Global evidence across multiple pandemic waves. PLOS ONE. 2021;16(7):e0253116. doi:10.1371/journal.pone.0253116
- Paroni L, D’Apice C, Ussai S, et al. The Traffic Light Approach: Indicators and Algorithms to Identify Covid-19 Epidemic Risk Across Italian Regions. Front Public Health. 2021;9:650243-650243. doi:10.3389/fpubh.2021.650243
- Han E, Tan MMJ, Turk E, et al. Lessons learnt from easing Covid-19 restrictions: an analysis of countries and regions in Asia Pacific and Europe. The Lancet. 2020;396(10261):1525-1534. doi:10.1016/s0140-6736(20)32007-9
- Kleczkowski A. Did the Covid lockdowns work? Here’s what we know two years on. The Conversation. 25th of April 2022.
- Sample I, Grover N. South African Covid-19 variant has reached the UK, says Matt Hancock. The Guardian. Accessed 25th April 2022.
- Mehta N, Shukla S. Pandemic Analytics: How Countries are Leveraging Big Data Analytics and Artificial Intelligence to Fight Covid-19? SN computer science. 2022;3(1):54. doi:10.1007/s42979-021-00923-y
- Editorial. This is no time to stop tracking Covid-19. Nature. 2022;603(550)
- Tao S, Bragazzi NL, Wu J, Mellado B, Kong JD. Harnessing Artificial Intelligence to assess the impact of nonpharmaceutical interventions on the second wave of the Coronavirus Disease 2019 pandemic across the world. Sci Rep. Jan 18, 2022;12(1):944. doi:10.1038/s41598-021-04731-5
Dr Arvinder Singh is a PhD Fellow in the Community Health Department at Universiti Kebangsaan Malaysia).








