The Ministry of Health (MOH) has reported 19,099 fewer deaths for the period from March 2020 to June 2021, when compared to the pre-pandemic period of 2015 to 2019.
The researchers attributed these negative excess mortalities to the decline in non-communicable diseases (NCD), namely ischemic heart diseases (IHD), chronic obstructive airway diseases (COAD), diabetes mellitus (DM), and cerebrovascular accidents (CVA) and acute respiratory infections, namely pneumonias.
It was proposed that the lockdowns have had a positive effect on the lifestyles of citizens, namely on food intake and the fact that more time is spent at home.
However, the proliferation of food delivery services would tend to favour unhealthy culinary habits, and being restricted in the home would only increase the risks associated with a sedentary lifestyle. We would suggest that the reduction in mortality is mainly due to the decrease in transmission of respiratory pathogens.
The World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC) have acknowledged, albeit belatedly, that Covid-19 is airborne, and we would like to think that the non-pharmacological interventions (NPI), namely lockdowns, masking, and physical distancing have virtually sanitised the planet and made the air much cleaner, fresher, and relatively free from respiratory pathogens, apart from the coronavirus.
Apart from mitigating the deleterious dispersion of the coronavirus, it also had the effect of reducing the spread of other airborne pathogens. In children, we witnessed a dramatic reduction of respiratory syncytial virus (RSV) bronchiolitis, para-influenzae acute laryngo-tracheo-bronchitis, meta-pneumovirus acute respiratory infections, and influenza pneumonias.
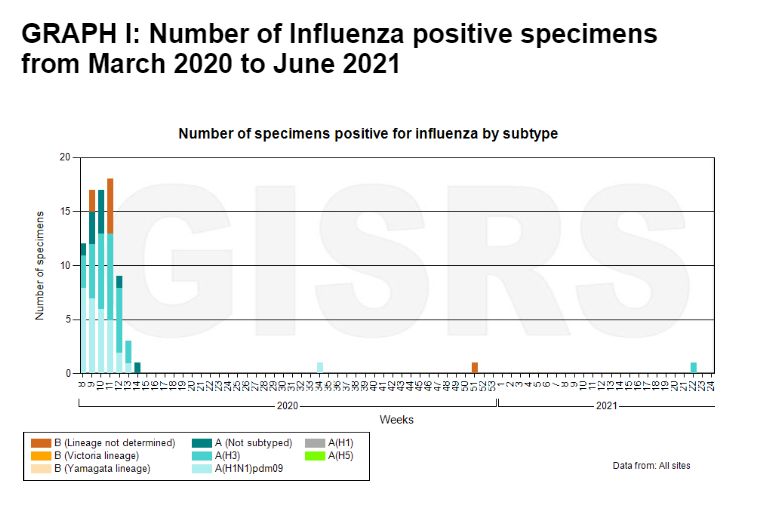
Besides the first four epidemiology weeks of March 2020, there were virtually zero influenza viruses circulating, as illustrated by Graph I below.
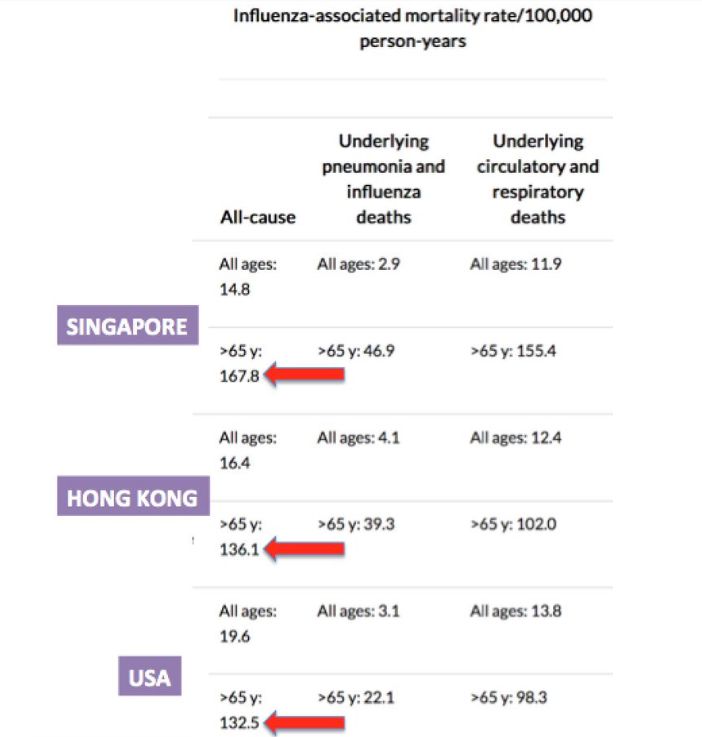
Adults, the elderly above 65, and those with chronic diseases like the various NCDs, are high-risk groups for influenza.
Following hospitalisation due to influenza, seven out of 10 persons more than 65 are at higher risk of developing complications such as pneumonia (second leading case of death in Malaysia), inflammation of the heart, inflammation of the brain, sepsis, and multi-organ failure. 85 per cent of flu-related deaths occur in people above 65.
Influenza exacerbates pre-existing conditions. The influenza virus was detected in up to 28 per cent of COAD patients, who have a higher risk (six times) of myocardial infarction within the first seven days of confirmed influenza. And with influenza, diabetics are six times more likely to be hospitalised.
Nine out of 10 patients who were hospitalised with influenza had at least one chronic condition. The risk of flu-related death increases 20 times, five times, and three times if one has heart and pulmonary diseases, heart disease, and diabetes, respectively.
During the period between March 2020 and June 2021, high-risk children, the elderly above 65, and those with comorbidities were spared of the scourge of the influenza virus. This, we think, contributed considerably to the 19,099 fewer deaths during this 18-month period.
Contrast this with the pre-pandemic period from October to December 2019, when Malaysia recorded 1,015 more deaths compared to the same period in the three-year average (2016-2018) as shown in Graphs II and III.
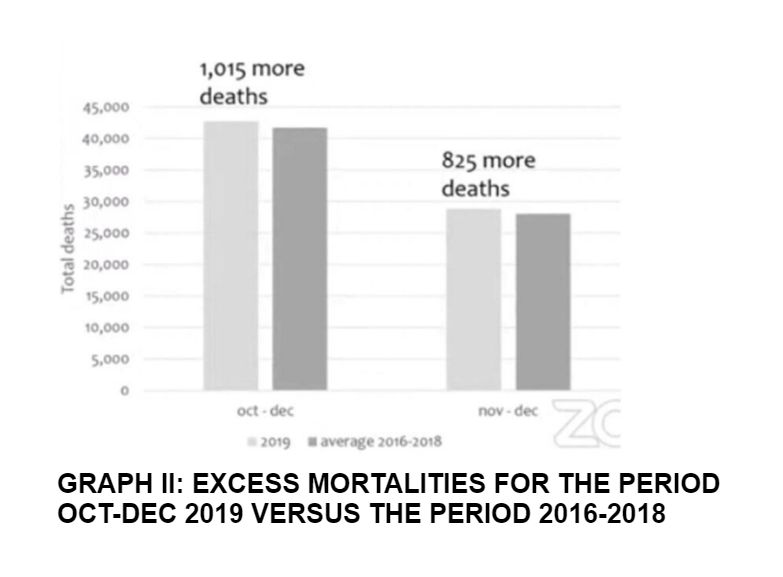
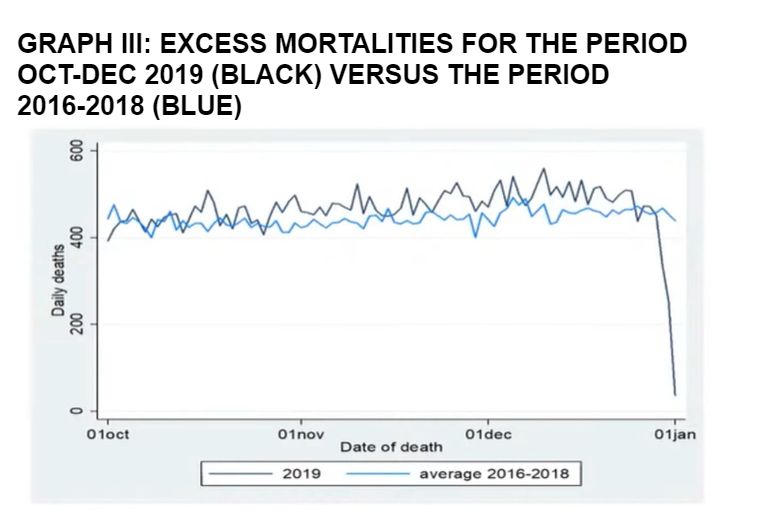
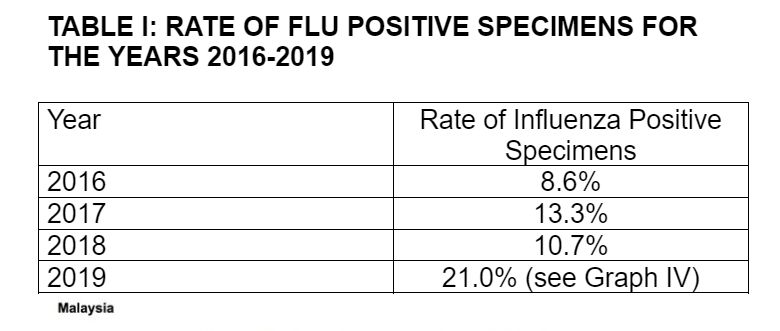
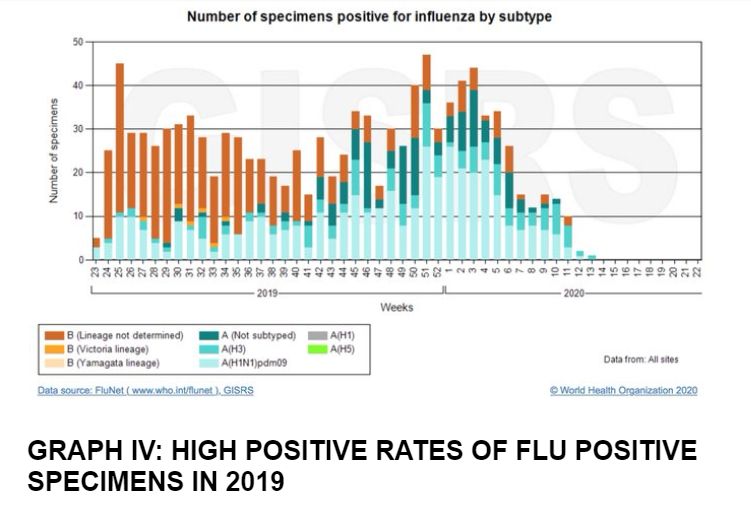
To validate that these excess mortalities were related to the influenza virus, we checked the rate of flu-positive specimens during the respective periods on Flu-Net.
Every one in five specimens collected from our national sites in 2019 was positive for the influenza virus (21 per cent), nearly 1.6 to 2.4 times the incidence from 2016 to 2018. (Table I)
The influenza-associated mortalities rates per 100,000 person years in Singapore (no Malaysian data available) is 167.8 for those more than 65 versus 14.8 for all ages. This is 11 times more, and explains the excess mortalities in older persons above 65. (Graph V)
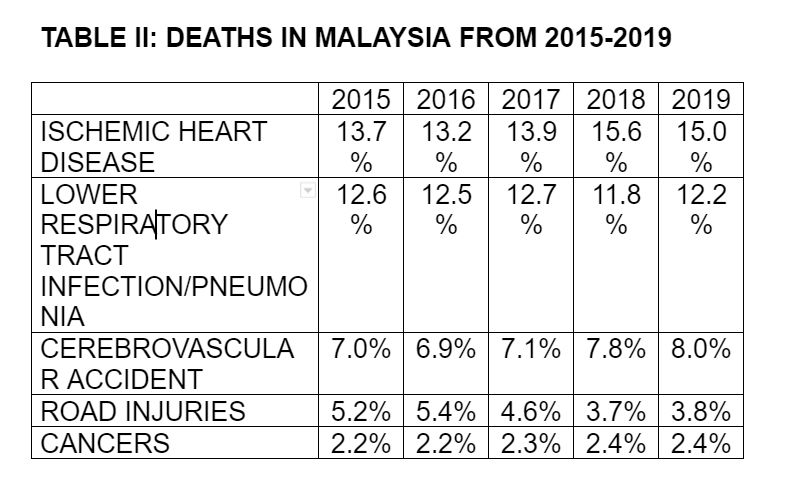
There are probably other reasons for the negative excess mortalities. This includes lower numbers of vehicles on the road, leading to less motor-vehicle accidents (MVA) and deaths due to traffic injuries. Looking at previous figures, deaths due to traffic injuries represented 3.8 per cent of deaths versus 15 per cent and 12.2 per cent due to IHD and pneumonia deaths respectively in 2019. (Table II)
With the lifting of lockdowns and the relaxation of masking and physical distancing mandates, we are beginning to see an upsurge in circulating flu virus and influenza cases. Graph VI shows positive specimens for influenza from January 2019 to April 2022. (Influenza is making a comeback-Protect your patients in the “New-Normal”. Musa Mohd Nordin, Husna Musa. e-Berita MMA. April 2022)
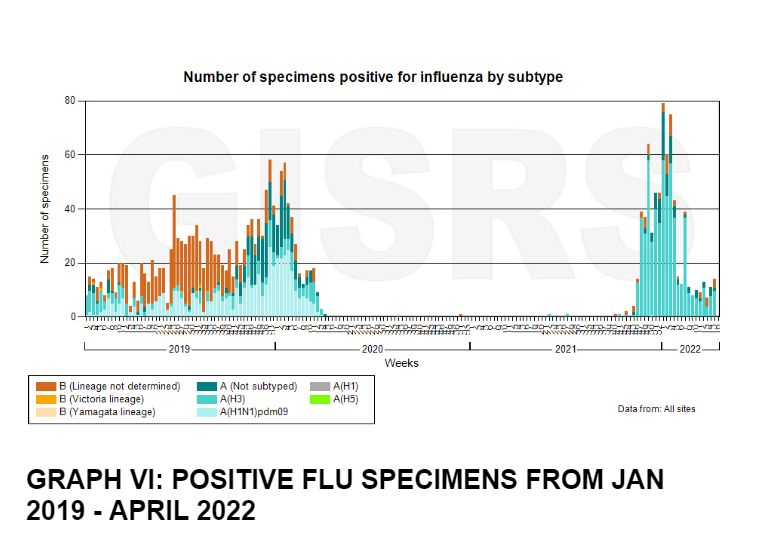
It is therefore of utmost urgency that the MOH address this upsurge in influenza proactively. The most effective way to prevent the flu is by getting the flu shot.
The influenza vaccine has been shown to reduce the severity of symptoms, reduce the risk of major cardiovascular events by 36 per cent, reduce the risk of hospitalisation by 45 per cent, reduce the risk of death by 42 per cent, and protect the independence of the elderly.
In the United States, seasonal flu costs the economy around US$90 billion. In Malaysia, influenza occurs throughout the year due to the nature of our climate and environment, making it difficult for predictive modelling trends, which means that we need to stay vigilant throughout the year. Surely one is unable to do so over long periods of time, thus making the case to ensure protection through influenza vaccination even more compelling.
We would strongly advocate for the influenza vaccine to be included in the National Immunisation Programme in order to protect the elderly above 60. We would also advocate that health care providers urge high-risk groups to get their flu shots.
These includes infants and children, pregnant women, those with comorbidities, travellers (including those doing the umrah and hajj), and not forgetting health care workers themselves.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.



