I was planning to have a quiet Christmas and year-end. I have written more than 40 articles on the Covid-19 pandemic since January 2020, had numerous media interviews, and worked on many statements with the Malaysian Health Coalition (MHC) and other groups.
I needed a break, and had turned away a number of media requests. But three recent events, like the proverbial straws that broke the camel’s back, have galvanised me to share my opinion.
I’m trying here to offer an honest and evidence-based assessment of our Covid-19 response for the last two years.
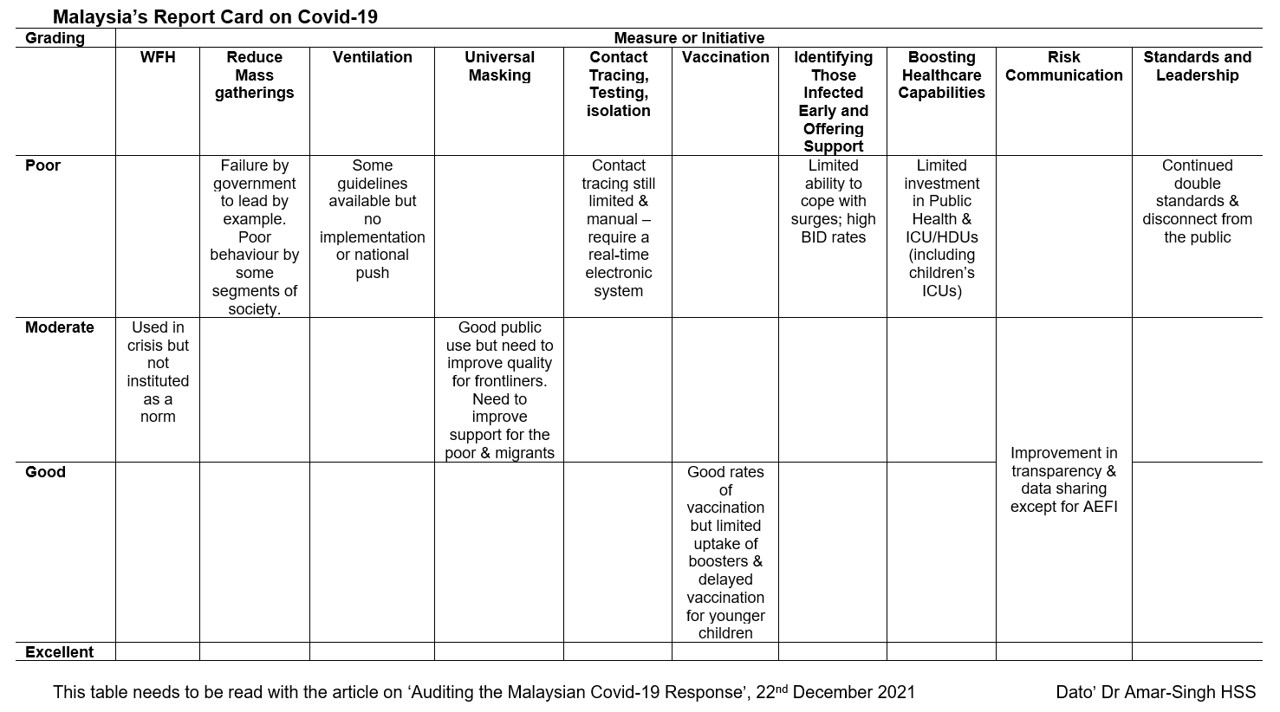
I ask myself this question: “Are we ready for the Omicron and other variants that are coming our way?” This article is a report card (see above image) of the government’s responses and its current measures.
Allow me to start by describing the three recent events that have distressed me, and highlighted how unprepared we are as a nation.
Firstly, we are all aware of the recent attempt to pass Act 342 to increase the penalty on those who violate SOPs. The magnitude of the fines and imprisonment, and the speed at which it was being pushed was totally unacceptable, when considering the fact that the largest rule-breakers are those in government, or VIPs who get away almost scot-free.
Fortunately, the enormous public outcry and the receptiveness of the health minister have seen this bill being postponed, and hopefully, be revised accordingly.
Secondly, the 100-day Keluarga Malaysia celebration by the government, while breaking SOPs, was disgraceful. The government is expected to set an example for the people.
Instead, they organised a mass event that could spread Covid-19, attended by more than 100,000 people.
The numerous messages all of us received to attend the event, even after it was clearly recognised as dangerous, and the lack of urgency to shut it down immediately speaks of no Covid-Sense by the government.
They have failed to learn the key issues regarding the spread of Covid-19 that many Malaysians already know.
Finally, I would like to talk about a personal matter. In mid-November 2021, I was invited to attend a Parliamentary Select Committee (PSC) hearing to assist in a review of the government’s approach towards Covid-19 since the beginning — to identify issues, strengths, and weaknesses, so as to prepare ourselves for future pandemics.
I was fully agreeable to support such an initiative, but I was also aware that the parliament building has not had significant improvements in ventilation. Therefore, I offered to do the session virtually.
I was surprised to be informed that, due to Parliament Standing Orders, I could only offer my opinion by being physically present in Parliament. There are concerns that the hearing would be considered as confidential (Akta Rahsia), and that online conversations could be recorded.
I then offered to write my opinion in an extensive, detailed report, but this was also not acceptable. Those attending Parliament have been relying on weekly PCR or Rapid-Ag tests to ensure safety.
But note that during the November 2021 Dewan Rakyat sitting, 84 infections were identified. If the august Parliament building has not had its ventilation significantly improved, and the proceedings have not moved online, what hope is there for the rest of the country?
They can opt for an expensive measure like frequent testing, but this is not an option for the average Malaysian.
Allow me now to use available evidence and internationally recognised best practices to benchmark our performance and current preparedness.
This will be a summary of our current preparedness, and I have categorised them under key issues. It is important to remember that vaccination is just one aspect of the Covid-19 response, and many other measures are equally important.
Prevention of Covid-19 (Stay Away From The Virus)
The best measure against Covid-19 is prevention, which include work-from-home arrangements, border controls, and the reduction of mass gatherings. I will not speak about border controls, except to say that current evidence does not support their use.
1. Work-From-Home (WFH) Arrangements
There has been limited use of this valuable strategy. It has been put in place when we have had major spikes in cases, but the government has not advocated for routine WFH when the job makes this possible, both for those in the civil service and the private sector.
Employers and heads of departments are of the opinion that their staff members do not work as much at home, and as such, has demanded they return to the office.
If we ever want to live with Covid, enter an endemic phase, or deal with new pandemics, WFH will be a useful measure.
Score: Moderate
2. Reduction Of Mass Gatherings
We are all conscious of the need to maintain physical distancing, but numerous recent events have shown a failure by the government to lead by example.
In addition, some segments of society have limited understanding of the risks, and continue to exhibit poor behaviour.
Any gathering where food is served will pose a major risk, especially if held indoors, or with large crowds outdoors.
We need to rethink how we conduct our marriages, funerals, and festive occasions. As World Health Organization (WHO) director-general Dr Tedros Adhanom Ghebreyesus said regarding the Omicron variant and year-end festivals, “An event cancelled is better than a life cancelled”.
Score: Poor
Risk Reduction (Mitigation Measures To Reduce Viral Loads)
The second best approach to deal with Covid-19 is to reduce your viral load and risk. This can be done by improving indoor ventilation, wearing good masks and contact tracing.
These must become sustainable lifestyle changes in society that should continue beyond the current pandemic.
1. Ventilation And Outdoor Activities
We are fully aware that the virus is airborne, and that this is the primary and most important mechanism of infection. Any amount of physical distancing in a closed indoor environment is of limited value, without significant improvements in ventilation.
Sadly, we have yet to make any major impact in this area, despite the drawing up of national guidelines. The few government departments we have visited (for critical purposes) in the last two months have not changed their ventilation practices.
Doors and windows remain closed, there is no appreciable change to the air-conditioning filtration system, there are no reliable portable air cleaners in use, and there are no reliable CO2 monitors available.
The staff seemed oblivious to the need to improve ventilation. Offices, restaurants, food outlets, and supermarkets do not appear to have changed their ventilation systems yet (limited outdoor seating for restaurants).
Schools that have changed their ventilation system have done so on their own initiatives. The risk communication to the public about airborne Covid-19 and ventilation remains poor.
Score: Poor
2. Mask Mandate
Masks are a critical element in preventing the spread of this airborne pandemic. It is vital that we improve the quality of fit and filtration of masks worn by frontline personnel, including doctors, nurses, pharmacists working in health clinics, police personnel, those working at food outlets and supermarkets, teachers, etc.
While the Ministry of Health (MOH) has provided N95 masks to those working in Covid-19 wards or high-risk areas, we have not changed the mask situation for those working in health clinic settings.
A surgical mask (or even a double mask) is inadequate for frontline personnel, especially in the face of both the Delta and Omicron variants. We need to provide them with FFP2 equivalent masks or KF94.
The general public has been good at mask use, but not VIPs, ministers, and even lawmakers in Parliament, who often take off their masks to speak.
Mask support for those who are poor has been limited. Currently, they still struggle to maintain SOPs, purely because of a resource-limited reason.
In March 2020, the then-Prime Minister, via the National Security Council, announced that 10 million masks will be imported from China, and be distributed to all Malaysians who need it.
The National Disaster Management Agency (Nadma) was tasked to use its allocation provided by the government to fund this. One wonders what has happened to this initiative, and the financial allocations for it.
Score: Moderate
3. Contact Tracing, Testing, Isolation
In the past month, the MOH has launched a national testing strategy, which health experts have long called for.
But this is not accompanied by a robust IT infrastructure with near-real time alerts for citizens. We need an automated case notification system that is linked to epidemiological investigations, home case monitoring, and health facility response planning and preparedness.
Our health care staff have long gone past the point of exhaustion, and have failed with manual contact tracing. In the face of Omicron with a doubling time of 1.5 to 2.5 days, conventional contact tracing and testing will not work.
Frequent testing is still out of reach for the average Malaysian, despite some initiatives by the health minister to reduce the prices of testing kits. The United Kingdom example of free (government-subsidised) testing kits is critical for the poor, schools, and for many businesses that are struggling.
In recent months, the new health minister has announced the allocation of tangible resources for the poor (rapid test kits, reusable face masks, pulse oximeter), but they will require ongoing support.
Home isolation has also been fraught with limited supervision and support.
Score: Poor
Reduce Severity (Reduce The Severity Of Damage By Covid-19)
The third approach to dealing with Covid-19 is to put in place measures that limit how much damage will occur, if one gets infected. These include vaccination, early identification, support of patients, and improving the health fitness level of the general population.
I will not comment much about the general health fitness level of the community, except to say that data suggests it has generally deteriorated (higher obesity rates).
1. Vaccination
Vaccinations are a key component in bringing the Covid-19 pandemic under control. While we had a slow start to vaccination due to supply issues, we have rapidly improved.
It was impressive how quickly we vaccinated both the adult and the adolescent populations. Sadly, this same impetus has not been seen with boosters, due to community concerns with side effects and mixing boosters, and the propagation of fake news.
There was an initial unacceptable disparity in vaccination supply between states, which left some regions less well protected initially, especially Sabah.
It is important to note that we should have avoided PPVs (mega vaccination centres), as the data suggest they are potential sites for Covid-19 spread.
We should have relied on, and utilised, existing health care infrastructure, including maternal and child health clinics, school health teams, GP clinics, and private hospitals.
While we are done with vaccinating adolescents, vaccine supplies for children aged 5 to 11 is only expected to arrive in June 2022. This is far too late, and we should seriously consider using existing vaccine formulations at lower doses, with parental consent.
Score: Good
2. Identifying Those Infected Early and Offering Support
During the surge in local cases, the health care system was overrun, and was unable to cope. Test positivity rates exceeded 15 to 20 per cent, brought-in-dead (BID) rates were as high as 20 to 30 per cent, and many could not be placed in limited ICU wards.
There was no ability to cope with the surge capacity until the Greater Klang Valley Special Task Force (GKVSTF) was created to focus on the issue, with significant support from the army.
The health care system continues to be at risk of being overrun, and the current BID rate is still high at 8 to 9 per cent. There were states where the health care services did better, especially Sarawak and Perak due to good leadership by state governments or health care workers.
Score: Poor
Supportive Measure (Health Services and Society)
There is another group of measures we need to look at. These include support for the health care services, support for the public, and leadership.
1. Support For Health Care Workers, Health Infrastructure, And Resources
The support for our health care workers and health infrastructure and resources is still limited. Funding, manpower, and infrastructure have seen very poor growth during the past 20 to 30 years.
The pandemic has revealed how governments of the past 30 years have failed to adequately invest in the health care system. In addition, health care workers do not feel adequately supported.
The lack of resolution of the contract medical officer problem after so many years shows the lack of interest in improving the health care services.
We need to work to keep our health care workers, since we are losing doctors to the private sector and other countries because we do not support them.
The physical infrastructure (adult and paediatric ICUs) needs a major overhaul. Our surveillance infrastructure needs massive investment. Our genome testing is very weak, compared to other countries which are at our level of development.
Score: Poor
2. Risk Communication And Data Transparency
Our risk communication was initially limited, with a serious trust deficit.
The development of the excellent CovidNow website by volunteers aided by MOH, and the data shared on GitHub have helped to restore some confidence in the system.
However, the lack of adequate communication about vaccine side effects (AEFI), the lack of data transparency on vaccine side effects, and the lack of an easy mechanism to collect data on vaccine side effects have fuelled a flood of fake news reports on WhatsApp and Telegram groups. This has damaged the credibility of the national vaccination programme.
We should offer honest and transparent local data on vaccine side effects to the public, and admit that there are rare serious side effects.
Only good, honest, transparent risk communication will support vaccine and booster-hesitant individuals, which is currently the major challenge.
Score: Moderate to Good
3. Standards And Leadership
The continual double standards practised by those in government and VIPs, compared to the average person on the street, has hampered our Covid-19 prevention programme.
Punitive actions against those who are poorer, compared to the rich and powerful, show a lack of compassion, and a selective use of legislation. This has resulted in the recent outpouring of anger against the amendments to Act 342, which were perceived as further victimising the average Malaysian.
Some wise decisions were the appointment of Khairy Jamaluddin as the health minister, and the formation of the GKVSTF.
Score: Poor
The Covid-19 pandemic is far from over, with the continuing spread of the Delta variant, and the threat of Omicron and other variants. The rakyat recognise that we are in this together, and most are trying their best to be responsible.
It is high time that the authorities work closer with the people, and play an improved supporting role.
Humility in the face of the changing landscape of the pandemic is what will see us through. Good leadership is key, and we are sorely lacking anything resembling such a thing.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.