About a week ago I wrote an article, Prepare for the Delta Wave of Covid-19 Outside the Klang Valley to highlight the deteriorating situation in some states. This article is to share the reality, and the crisis that is already upon us.
Situational Analysis
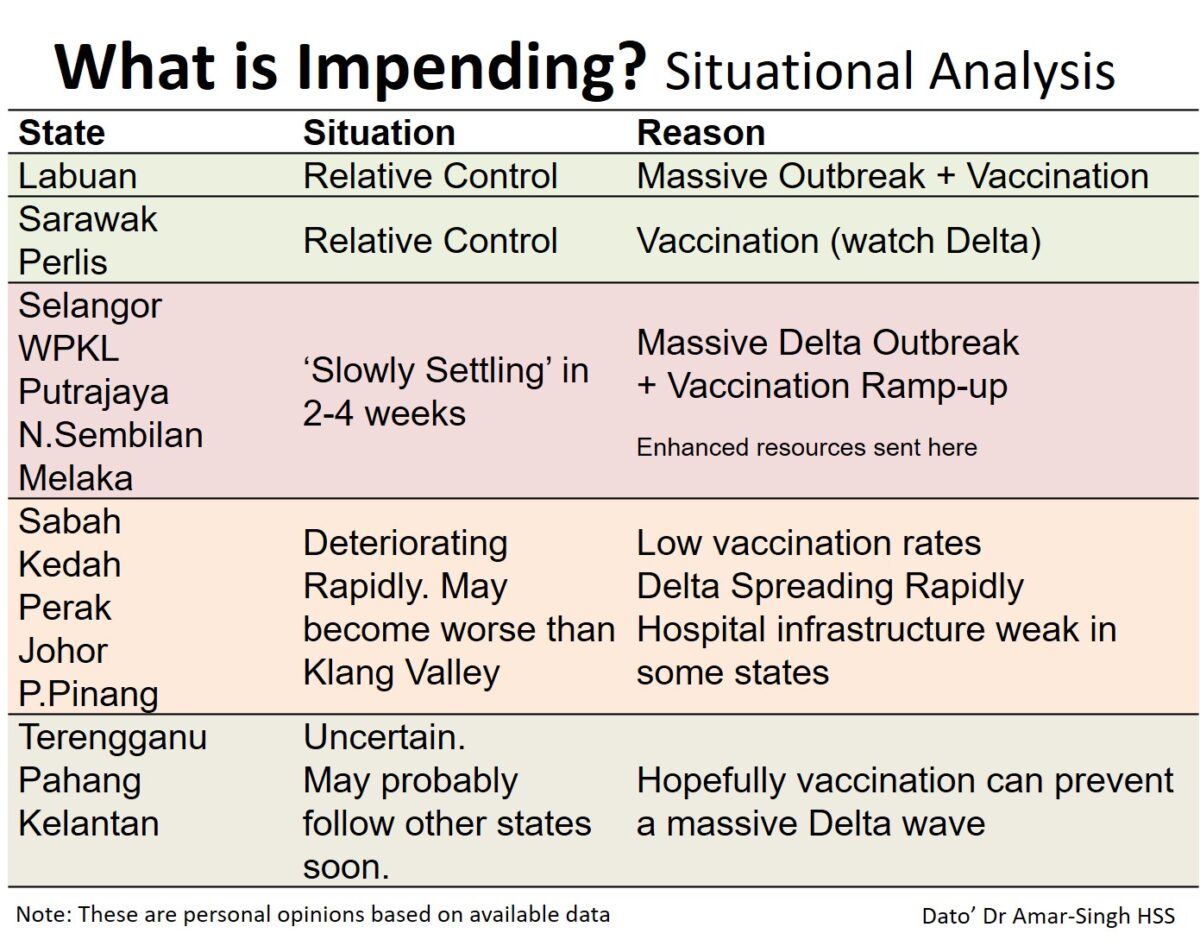
The graphic below shows the situational analysis of what is potentially impending for different states. The crisis situation in the Greater Klang Valley (Selangor, Kuala Lumpur, Putrajaya and Negeri Sembilan) will probably slowly settle down over the next two to four weeks, due to the huge Delta outbreak, massive vaccination ramp-up, and enhanced resources poured in by the government and civil society.
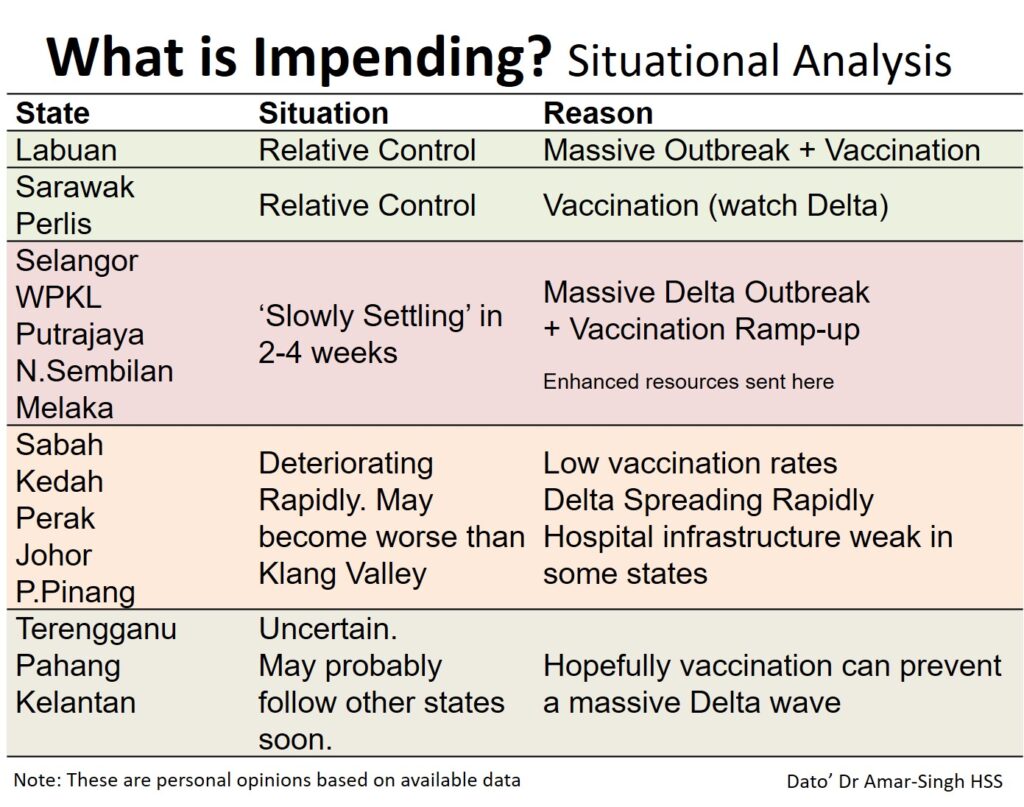
However, total numbers in the country and even deaths may not come down as the Delta wave hits other states hard, especially Sabah, Kedah, Perak, Johor and Pulau Pinang.
These states are deteriorating rapidly, and may become even worse than the Klang Valley as they have low vaccination rates (due to low vaccine supply), and some have weak medical infrastructures (especially Sabah). All these states have second-dose (completed) vaccination rates of under 20 per cent.
The table below shows the ICU bed usage for these five states. It is important as we look at this data to understand the reality.
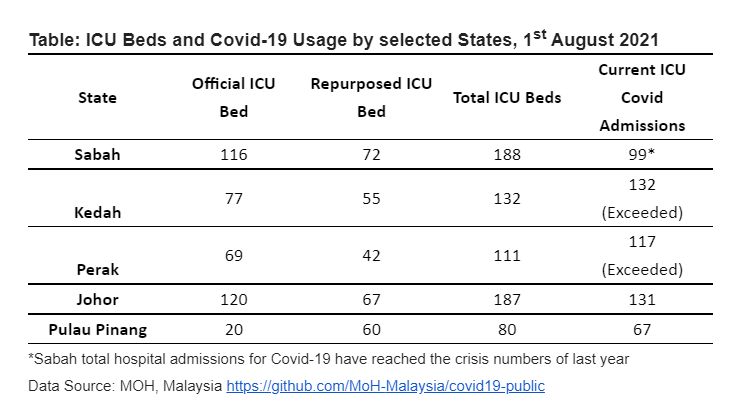
- The trend of ICU bed usage for July is on a steep upward curve.
- Almost all have exceeded their official ICU bed numbers. These are the original ICU beds they have, and are of far better quality than repurposed ICU beds.
- Kedah and Perak have exceeded their total ICU beds (original and repurposed beds), and are in full crisis mode.
- Sabah may ‘look’ better, but its total hospital admissions for Covid-19 have matched the crisis numbers from last year. Hospitals are struggling to cope.
- Remember that these numbers do not take into account patients who should be in ICUs (Categories Four and Five), but are being managed in emergency departments and quarantine centres. Kedah also has a high number of brought-in-dead (BID) patients.
We Can Never Be Prepared Enough For Delta
We need an all-of-society approach to deal with the crisis as it grows.
I would like to make some suggestions for the health departments, state governments, corporate bodies, civil society and the general public. More details can be found in the Health Emergency Action Plan: Roadmap to Recovery from Covid-19 we recently devised.
1. Reality-based data sharing of the situation by state health departments.
It is vital that the public in each crisis state (Sabah, Kedah, Perak, Johor and Penang) be aware of the full reality.
The time for statements like “Don’t worry, everything is ok”, “We are in control of the situation”, or “We have prepared for this crisis” is past; these statements are of no value. Delta does not respect or care about these attempts to ‘not alarm’ the public.
We can never be prepared enough for Delta and the Klang Valley, with all its resources, shows this clearly. State health departments must have daily crisis sharing with the public (through the mainstream media and social media). Trust and transparency are crucial to fighting the pandemic.
2. State-level disaster management teams led by state Health directors, fully supported fully by state governments. and withstrong engagement with corporate bodies and civil society (NGOs).
Those of us outside of the Klang Valley know that no help is coming for our states. The federal government has limited funds, having invested significant resources to support the Klang Valley.
Therefore, we must work very closely with business leaders and NGOs to ramp up resources and services. We need strong, decisive leadership, and not individuals from the state administration looking gain financially from the crisis.
3. Don’t put all our eggs in the vaccine basket.
While we advocate for more vaccine supply and ramp up vaccination, we must not put our hopes on vaccination alone.
We need to use good public-health measures such as proper masking, avoiding all unnecessary social interaction, effective contact tracing, and using RTK-Ag testing for confirmation, all of which the World Health Organization (WHO) has been advocating.
Lockdowns are not the solution. The continued use of mega vaccination centres (PPVs) runs the risk for large-scale Covid-19 transmissions. We should fully transition to using health clinics, school health teams, general practitioners, private hospitals, and outreach teams for vaccination.
What Can Corporate Bodies, Civil Society (NGOs) And The Public Do To Support Their States?
1. Purchase and donate equipment to hospitals and quarantine centres.
Corporate bodies, NGOs and the public should liaise directly with medical specialists and medical offers to find out about the real needs on the ground. They will specify the items needed and where to get them.
Some important items include oxygen concentrators, oxygen tanks, oxygen regulators, infusion pumps (to deliver drugs), portable suction machines, portable vital sign monitors, blood-pressure monitoring sets, ECG machines, stretchers, and canvas beds.
Ensure the Personal Protective Equipment (PPE) that health care workers are wearing are of good quality, including N95 masks, powered air-purifying respirators (PAPR), isolation gowns, face shields, goggles, gloves, disposable caps, and footwear.
Provide Medical Device Authority (MDA) approved RTK-Ag saliva test kits to enable health care workers to speed up and increase testing of all contacts within clusters and the community.
Consider offering reliable emergency transport services, since the public hospitals’ ambulance services will be overrun. This may help to reduce BID cases.
Increase ICU capacity by creating new ICUs — this requires arge corporate bodies to fund and rapidly construct (within two to four weeks) purpose-built ICU facilities at major hospitals.
2. Support Covid-positive individuals and contacts
Individuals who are Covid-positive or are close contacts will be required to home-isolate or be admitted to quarantine facilities. Those in home isolation will require reliable finger pulse oxymeters, medical support (daily video calls with health care workers), practical support such as meals, and RTK-Ag saliva self-testing kits.
Quarantine facilities for those that do not have accommodation suitable for home isolation (e.g. crowded homes, limited space, migrants, etc.). This would mean using hostels and hotels to house them, with individual rooms that have good ventilation and no central air conditioning.
3. Support communities hit economically by the pandemic
A significant portion of the public is struggling with daily needs, and we need to support them. Although government agencies are doing what they can, many have fallen through the cracks and have minimal support.
Partner with reliable local NGOs and disaster organisations that are delivering foodstuffs to the poor, and are setting up and maintaining food banks.
Adopt poorer families for six to 12 months, and offer a fixed sum of money monthly to aid with groceries and utility bills.
Donate food coupons that can be redeemed at sundry shops or convenience stores.
Hire individuals who have lost jobs to work as volunteers to support others.
We also need to support families who have lost loved ones, who have lost jobs, and are struggling to cope emotionally. This includes children who have become temporary (both parents hospitalised) or permanent orphans.
I appeal to the state governments of Sabah, Kedah, Perak, Johor and Penang to be transparent so that extensive and comprehensive emergency actions can be taken by society to deal with the crisis at hand.
There are mothers and fathers, sisters and brothers who need to be saved in the coming weeks. Please let us not wait until we reach an acute, Klang Valley-level crisis status.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.