KUALA LUMPUR, May 6 — Radiosurgery is a precision-based outpatient procedure that is far more effective in treating brain cancer, without affecting cognitive and other functions, than conventional radiotherapy, Beacon Hospital found.
Beacon Hospital’s Oncology Centre, which is based in Petaling Jaya, Selangor, has treated over 100 brain cancer patients in the past year with TrueBeam Radiosurgery with HyperArc system from Varian Medical Systems.
The TrueBeam Radiosurgery with HyperArc system is a radiotherapy machine using advanced stereotactic technology that delivers a much faster and more accurate radiation dose, as compared to a conventional radiotherapy system.
Consultant clinical oncologist and medical director of Beacon Hospital, Dr Mohamed Ibrahim Abdul Wahid, explained that the Varian TrueBeam radiosurgery with HyperArc system enables a very fine beam of high radiation to focus on the tumour to eradicate it, while minimising damage to the surrounding tissue.
“The beam is focused so that the tumour gets a very high dose of radiation, but not beyond the tumour. The dose fall-off is rapid so the good cells get a smaller dose of radiation hence reducing the side effects,” Dr Ibrahim told CodeBlue.
Consultant neurosurgeon Dr Lee Foo Chiang said that for brain tumours, the procedure is called stereotactic radiosurgery (SRS), a non-surgical radiation therapy without making a surgical incision or using general anaesthesia.
“SRS works by distorting and destroying the deoxyribonucleic acid (DNA) of tumour cells, much the same way as other forms of radiation,” Dr Lee said.
“As a result, these cells lose their ability to reproduce and die.”
Besides that, Dr Lee said that this state-of-the-art technology acquired by Beacon Hospital in 2019 can be used to combat both intracranial and extracranial brain tumours.
“Besides treating metastatic brain tumours, SRS can also be used to treat benign tumours like meningiomas, acoustic neuromas, arteriovenous malformation, trigeminal neuralgia etc.”
Meanwhile, Dr Ibrahim said that the whole treatment requires a multidisciplinary team — a neurosurgeon, an oncologist, a physicist, and a radiologist.
“The neurosurgeons will help to outline the tumour, define where the tumour is, define the target, confirm protection / avoidance of critical structure like optic nerve brainstem and then after that, we will send it for calculation,” Dr Ibrahim told CodeBlue.
The TrueBeam system generates high-quality 3D images of the tumour 60 per cent faster. These images are then used to fine-tune a patient’s position prior and during treatment.
“Then, the physicists will have to do the calculations to optimise the beam and QA before treatment. The oncologist will have to determine that the plan is safe before approval and only then patient can proceed with treatment.”
Every 10 milliseconds throughout the entire treatment, the system performs accuracy checks.
Beacon Hospital consultant neurosurgeon Dr Chee Chee Pin said that most brain tumour treatments take only about 20 minutes using the HyperArc technology, including the time taken to position the patient and verify the images.
“There are significant reductions in treatment time. Fast, automated treatment delivery management software that significantly shortens the duration of sophisticated treatments involving different beam angles,” Dr Chee said.
The treatment gives big doses at a very small period of time, within five or 10 consecutive days, which gives an advantage of preventing the tumour from having the time to repair itself.
“If you spread it up to six, seven weeks because there’s a time interval between each treatment, the cancer cells can start to develop resistance. That’s why we give all in one go and there’s no time to repair itself,” consultant neurosurgeon Dr Chee said.
Patient Managed To Preserve Cognitive Function Post-Radiosurgery
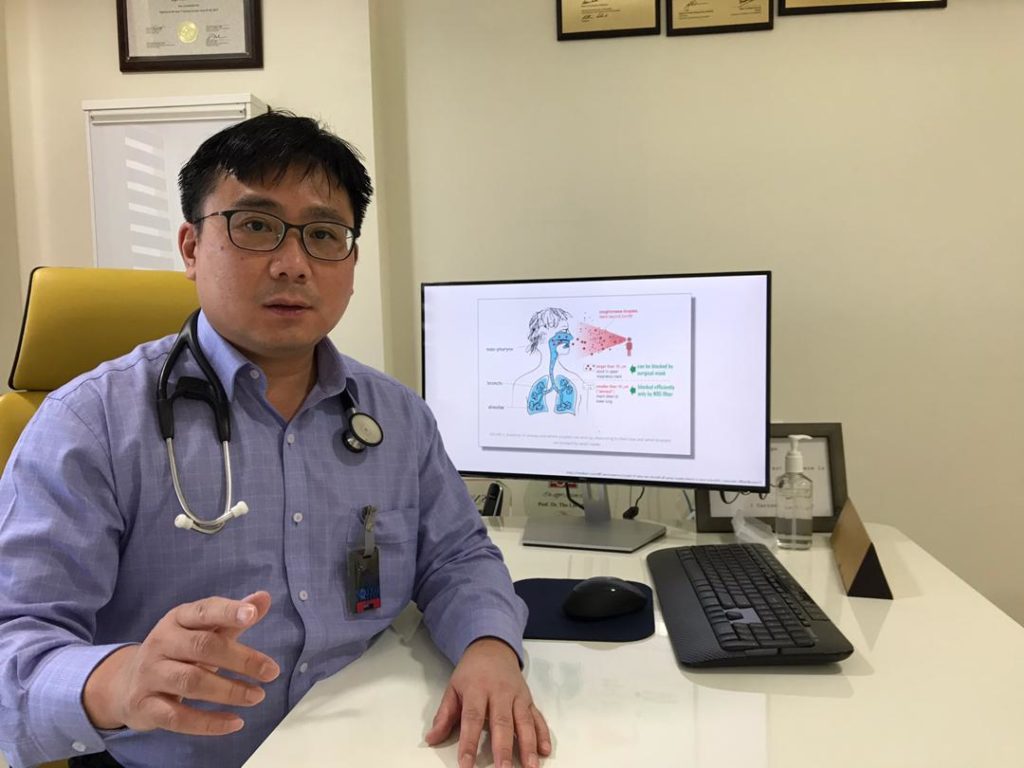
Consultant oncologist from Beacon Hospital, Dr Tho Lye Mun, shared that one of his former patients, who held a top position in a multinational company, managed to maintain excellent brain function after undergoing Varian TrueBeam radiosurgery.
“He had stage 4 lung cancer which had spread to the brain. So, we used stereotactic radiosurgery to target the tumour and kill it while avoiding the rest of his brain. Thus, he was able to maintain memory, thought processing and function, so he can not only continue to work, but also be able to have a good quality of life with his family,” Dr Tho said.
Dr Tho added that with Varian TrueBeam radiosurgery, the patient also did not have hair loss or significant side effects from the treatment, as opposed to conventional whole brain radiotherapy where patients could suffer hair loss, memory loss, and fatigue. Patients also do not suffer from skin burns or peeling, which is always a concern.
Nevertheless, some patients may experience mild and temporary dizziness and headache post-radiosurgery due to swelling, but this will usually subside.
“The main problem with radiosurgery is that swelling (also known as oedema) can also happen up to six months after radiation. If this does occur, then the patients will need to undergo a course of treatment to reduce swelling such as steroids or anti-angiogenic medication. This is all internal so you may not notice anything external,” Dr Tho added.
Moreover, the Varian TrueBeam radiosurgery can sometimes be conveniently delivered as an outpatient procedure, so patients don’t necessarily need to be admitted.
In dealing with brain metastases, the smaller the tumour, generally the better the success rate. Dr Tho added that for tumours smaller than 1cm, the control rate for radiosurgery is between 70 and 90 per cent, a much better outcome compared to conventional whole brain radiotherapy, which is only about 20 per cent successful.
”We want to catch and treat the tumour before they become big, so regular follow-up using MRI scans of the brain are generally recommended,” he said.
“We definitely do not want to wait until the tumour becomes so big and damaging that patients develop symptoms such as loss of function of their arm or leg or speech, which is the risk of not following up your patients carefully.”