We read this somewhat toxic article – “Proposed Medical Act Amendment ‘Huge Mistake’ With Non-Accredited Parallel Pathway: Paediatric Surgeon“, as published by CodeBlue – with mixed emotions.
We were blown away by senior consultant paediatric surgeon Dr Dayang Anita Abdul Aziz’s bravado to claim that it is a “huge mistake” by Health Minister Dzulkefly Ahmad to propose to the Cabinet an amendment to the Medical Act.
This is a new Malaysia and anyone can take a potshot at a minister; even the prime minister is not spared!
As Health Minister, Dzulkefly’s stewardship role is to produce more specialists for both the public and private health care sectors and to do it even better. It can only happen if he ensures the “feuding medical professionals” work together to enhance the quantity of specialists trained and jealously guard the quality of our medical postgraduates.
In the midst of the “hostile exchanges between the medical professionals”, the Health Minister has chosen to rise above the professional herd mindset, blindly protective of each other’s chosen career pathway.
Dzulkefly has elected to engage with the major stakeholders and to endeavour to harmonise the Parallel Pathway with the Masters programme and chart the future roadmap of our national medical postgraduate programme.
Even more astonishing is Dr Dayang’s naivete of the issues on the ground and their historical context.
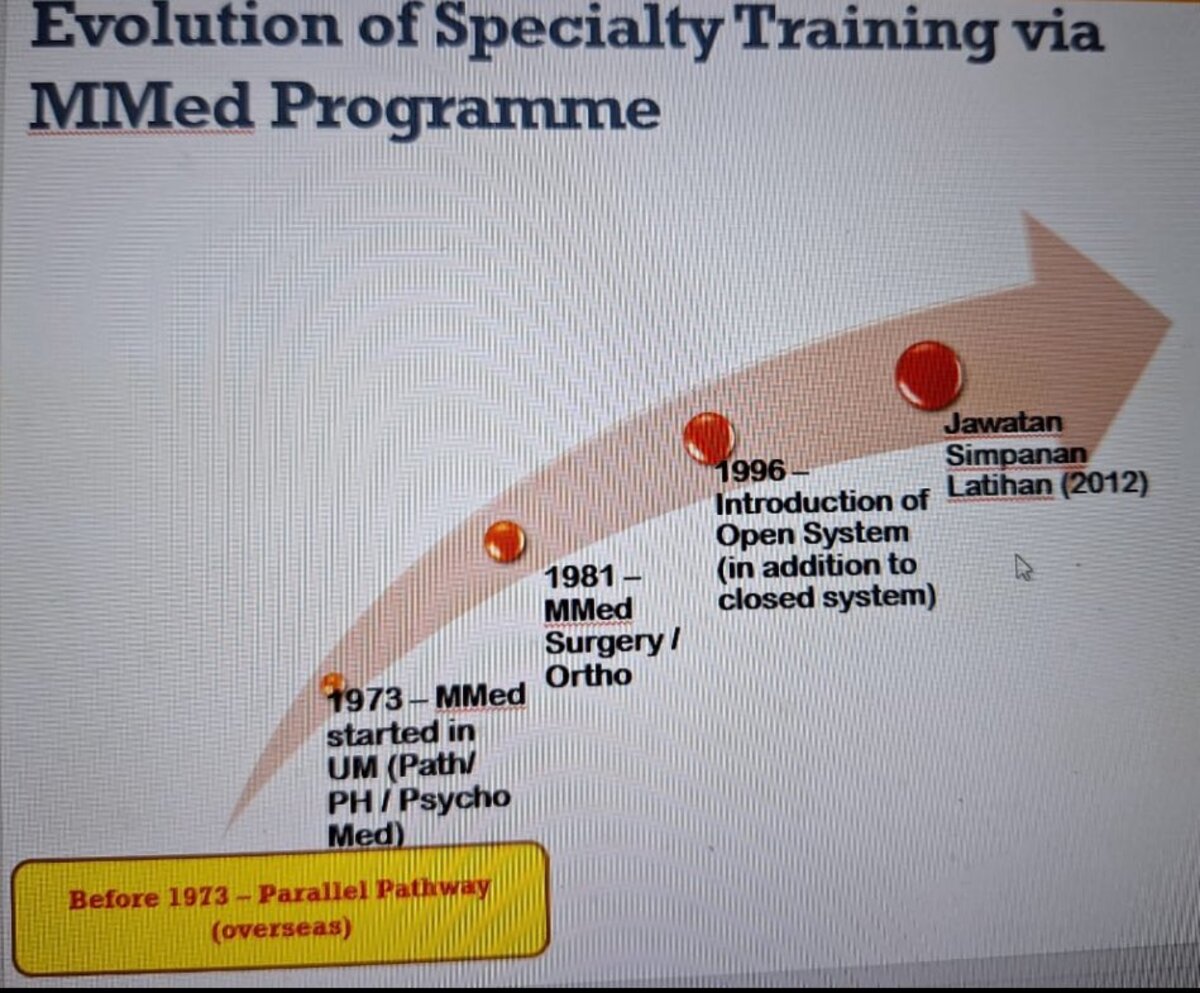
Prior to 1973, the Parallel Pathway was virtually the only trainer and supplier of the nation’s specialist manpower. Presently, there are 13 Parallel Pathway specialty training programmes in the Ministry of Health (MOH), with another five programmes in the pipeline.
Don’t we actually owe the Parallel Pathway a debt of gratitude for the many competent specialists it has produced, even before the Masters programmes took off?
The local Masters Medicine programme began in the University of Malaya in 1973, whereas the Masters Surgery and Orthopaedics programme started in 1981.
There are 25 Clinical Masters specialist training offered by our 11 public universities, and at least four other specialist training programmes offered by a private university.
The National Postgraduate Medical Curriculum (NPMC) was launched in 2021 by the Medical Deans Council to unify structured supervised training for both Masters and Parallel Specialist Training Pathways.
However, they are still insufficient to meet the public health care sector needs of 18,912 and 23,979 specialists in the years 2025 and 2030. At the present production rate, only 19 per cent of the total doctors in the public sector are specialists instead of the targeted 30 per cent.
As an example, the United Kingdom Royal College of Paediatrics & Child Health (RCPCH) formalised their work-based assessment in 2005; the paediatric Parallel Pathway in Malaysia followed suit in 2010.
Virtually all of the other Parallel Pathway programmes consolidated their curriculum, training, postings, work-based assessments, exit criteria etc since 2014.
To conflate the “issues of two to three surgical-based Pathway Programmes poorly managed by the Malaysian Medical Council (MMC)” to the other up and running successful Parallel Pathway programmes is totally uncalled for.
Instead, we wish to complement the arduous efforts on the ground to increase the numbers of highly trained medical experts to ensure high quality of the nation’s health care services.
Towards strengthening the medical specialist training programmes, all stakeholders – namely the MOH, Ministry of Higher Education (MOHE), MMC, the Academy of Medicine of Malaysia (AMM), private health care institutions etc – must abide by the Medical Act and training standards agreed upon.
They must endeavour to prioritise and strengthen the national postgraduate medical programme.
More recently, the MOHE and the Medical Deans Council of public universities hosted a pre-workshop meeting to discuss a framework of action on the overall direction and the way forward for specialist training in Malaysia.
The governance of the national postgraduate medical programme must address three pivotal issues, namely:
- Optimisation and recognition of specialist training places. There must be an online central registry of training centres, trainers, and trainees according to the various specialties.
- Documentation of a structured specialist training programme as outlined by the national medical postgraduate curriculum for both the Masters and Parallel Pathway.
- Completion of all specialist training pathways must be determined by an agreed set of exit criteria, which must be fulfilled by all the trainees prior to certification as a specialist by the National Specialist Register (NSR).
We need to find closure to this chronic imbroglio and, together, be part of the solution instead of being part of the problem!
As part of a just culture and our joint quest for excellence in health care, in God we trust, all else (Medical Act included) we audit, compassionately!
Dr Musa Mohd Nordin (KPJ Damansara Specialist Hospital); Dr Zulkifli Ismail (KPJ Selangor Specialist Hospital); Dr Erwin J Khoo (International Medical University); and Dr Timothy Cheng (Duchess of Kent Sandakan Hospital).
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.