The spread of respiratory disease has traditionally been thought to occur by the droplet route for large droplets, and aerosol or airborne route for small droplets.
The assumption in the former is that large droplets fall on surfaces or on others, leading to surface contamination. The assumption in the latter is that there is inhalation of pathogen-bearing droplets, which are smaller than 5 to 10 microns in diameter and are invisible to the naked eye.
“Whilst this conceptual framework of droplet size can be useful, the dichotomy between large droplets and small airborne particles emitted in isolation is an oversimplification. In fact, respiratory infections are transmitted via a continuum of droplet sizes embedded in a cloud of exhaled air containing those visible to the naked eye (millimetres), to invisible ones, in the micron scale.
“This droplet size continuum and the cloud that carries them have significant implications for mode of transmission. Social distancing rules are based on estimations of risk of droplet transmission in relation to isolated large droplet emission only.”
Whenever a person talks, coughs or even during breathing, tiny droplets are expelled into the surrounding air. The smallest of these droplets can float for hours with persuasive evidence that they can carry live coronavirus of an infected person.
The SARS-CoV-2 virus, which causes Covid-19, is currently believed to be spread by direct contact and droplets. However, the thinking that airborne spread of the virus by aerosols has increasingly gained prominence.
“Smaller airborne droplets laden with SARS-CoV-2 may spread up to 8 metres, concentrated in exhaled air from infected individuals, even without background ventilation or airflow. Whilst there is limited direct evidence that live SARS-CoV-2 is significantly spread via this route, there is no direct evidence that it is not spread this way.”
Aerosols and SARS-CoV-2
Aerosols are particles suspended in the air. When people breathe, talk, sing, cough or sneeze, the emitted respiratory droplets mix in the surrounding air and form aerosols. The larger droplets fall onto a surface rapidly.
On the other hand, respiratory aerosols, which are droplets less than 5 microns (about 1/10 the width of a human hair), form a sheet of liquid which breaks away. This event is illustrated by the blowing of soap bubbles, which sometimes do not form fully but breaks up into several droplets.
A similar event occurs in the respiratory tract with the airflow produced by breathing, speaking and coughing, breaking up the airway mucus, which are small sheets of liquid, just like blowing the soap bubble.
The droplet size produced depends on how and where they are produced in the airway. It has been shown that two to three minutes of talking can produce as many droplets as one cough.
Droplets smaller than 5 microns can remain suspended in the air for minutes to hours. Although the water content of a viral droplet evaporates, the droplet does not disappear. It becomes smaller and remains suspended in the air longer.
The risk of infection is increased as smaller droplets are more apt at deep penetration into the respiratory tract. It is of interest that the SARS-CoV-2 virus has been reported to be viable as an aerosol for up to three hours.
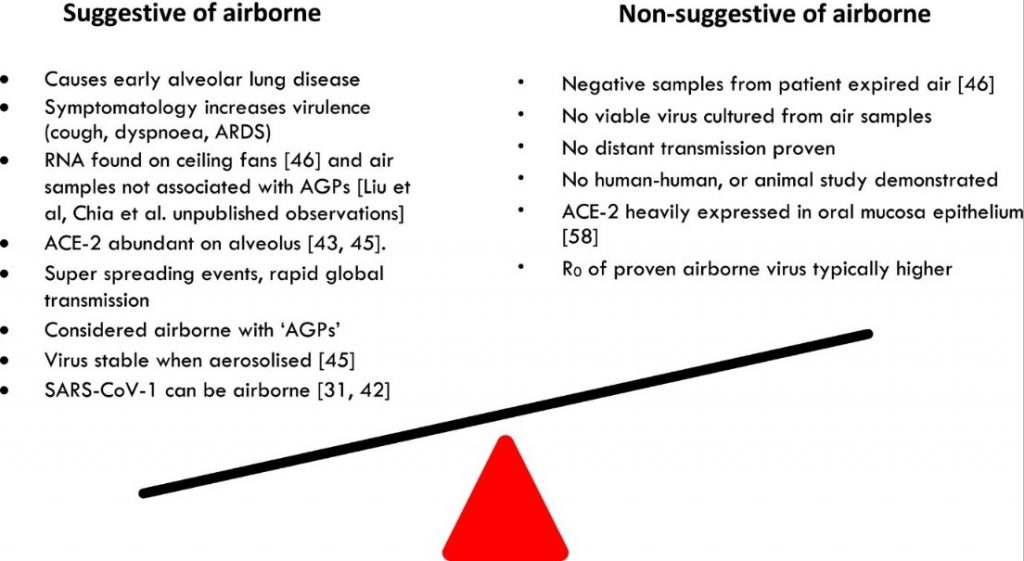
The current evidence for and against aerosol transmission of SARS-CoV-2 is summarised in the diagram below.
Protection from aerosol transmission
Face masks protect against aerosol transmission by filtering the air expelled by individuals, thereby preventing larger droplets from affecting another person directly or evaporating into a smaller size and then circulating in the air.
It also reduces the speed of the air expelled when talking, sneezing or coughing, thereby reducing the distance the droplets are transported into another person’s surroundings. It is essential to remember that protection from masks is variable, depending on the type and the manner of its usage.
The 2-metre physical distancing recommendation is based on a 1934 study that showed that an expelled water droplet either falls to the ground, or evaporates, within a distance of about 2 metres. However, the study did not take into account the fact that the viral droplet remains following evaporation of the water in it, thus still posing the risk of airborne infection.
As such, whilst the 2-metre physical distancing reduces exposure to the virus, it may not be enough in all situations, like an enclosed, crowded, poorly ventilated room.
Aerosol exposure indoors can be reduced by increased ventilation. However, air recirculation should be avoided unless there is effective prior filtration. The opening of doors and windows can increase fresh air flow.
The decrease in the number of people within a given space, particularly a poorly ventilated one, and the wearing of face masks at all times can reduce further aerosol exposure. The reduction of the duration spent in crowded, poorly ventilated areas is another way of reducing aerosol exposure risk.
The virus is deactivated in the operating theatre with disinfection wipes that contain a quaternary ammonium compound and alcohol; and use of germicidal ultraviolet light. Whether this is applicable in non-health care setting is another issue.
WHO position
The risk from aerosol spread of SARS-CoV-2 was not incorporated into the World Health Organization (“WHO”) guidelines until recently. The WHO’s position was that SARS-CoV-2 was spread primarily by coughing or sneezing large droplets onto someone’s face, rather than the virus hovering in the air, leading to a longer-term threat.
In an open letter to WHO on 6 July 2020, more than 200 scientists warned about the airborne spread of SARS-CoV-2 through aerosols and urged the WHO to recognize such risks. The letter stated: “Most public health organizations, including the WHO, do not recognize airborne transmission except for aerosol-generating procedures performed in healthcare settings…Hand-washing and social distancing are appropriate, but in our view, insufficient to provide protection from virus-carrying respiratory microdroplets released into the air by infected people.”
The WHO response was circumspect. Dr Benedetta Allegranzi, WHO’s technical lead for infection prevention and control, was reported to have stated: “There is some evidence emerging but is not definitive…The possibility of airborne transmission in public settings, especially in very specific conditions — crowded, closed, poorly ventilated settings — cannot be ruled out. However, the evidence needs to be gathered and interpreted.”
The WHO, in its 9 July 2020 document, “Transmission of SARS-CoV-2: implications for infection prevention precautions” stated: “Current evidence suggests that SARS-CoV-2 is primarily transmitted between people via respiratory droplets and contact routes – although aerosolization in medical settings where aerosol-generating procedures are used is also another possible mode of transmission…The role and extent of airborne transmission outside of health care facilities and in particular, in close settings with poor ventilation, also requires further study.”
“It may prove difficult to unequivocally establish whether SARS-CoV-2 is infectious when airborne due to technical difficulties associated with air sampling of viable viral particles, and human-to-human transmission being unethical”.
A 27 July 2020 report from Manchester University is illuminating: “Early results from a survey of 2,000 people in the UK and US has suggested that the Covid-19 transmitted through aerosol transmission is materially significant. The survey analysed by a team of data scientists in the UK, Norway and the US is one of the first to examine a wide range of personal and work-related predictors of transmission.
“Taking both samples together, being tall more than doubled the probability of having a Covid-19 medical diagnosis or positive test for people over 6 ft. The data in both countries, argue the researchers, could suggest that aerosol transmission is very likely, with taller individuals at higher risk – something that would not be expected if transmission was exclusively through droplets.”
The WHO did not initially endorse the use of face masks in infection prevention and control of SARS-CoV-2. This position was debunked when substantial evidence emerged to support the initial evidence.
It is to be hoped that the WHO will not ignore or take too long to acknowledge and increasingly persuasive evidence of aerosol transmission of the virus.
Summary
In summary: “Safe transmission mitigation measures depend on multiple factors related to both the individual and the environment, including viral load, duration of exposure, number of individuals, indoor versus outdoor settings, level of ventilation and whether face coverings are worn.
“Social distancing should be adapted and used alongside other strategies to reduce transmission, such as air hygiene, involving in part maximising and adapting ventilation to specific indoor spaces, effective hand washing, regular surface cleaning, face coverings where appropriate and prompt isolation of affected individuals.

Dr Milton Lum is a past President of the Federation of Private Medical Practitioners Associations, Malaysia and the Malaysian Medical Association. This article is not intended to replace, dictate or define evaluation by a qualified doctor. The views expressed do not represent that of any organization the writer is associated with.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.








