According to the National Health and Morbidity Survey (NHMS), the percentage of women who underwent cervical screening has increased from 26 per cent in 1996 to 43.7 per cent in 2006. However, as of 2011, this percentage has dropped to 12.8 per cent.
The World Health Organization (WHO) advocates that interventions such as HPV vaccination, cervical screening and proper treatment are imperative for the elimination of cervical cancer.
The 90-70-90 target outlined by WHO states that each country should target HPV vaccination in 90 per cent of girls by 15 years old, screening in 70 per cent of women by 35 years old and again at age 45, as well as treatment of 90 per cent of women identified with cervical disease by 2030.
Hence, this article will provide concise information about cervical screening in Malaysia, with emphasis on tests involved and where to access them.
What Is Cervical Cancer?
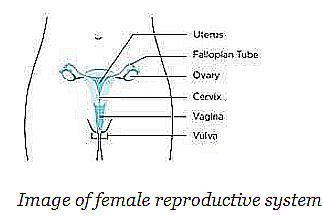
Cervical cancer is a disease where cells of the cervix grow uncontrollably. The cervix connects the birth canal to the womb as illustrated above.
In Malaysia, cervical cancer is among the top 10 cancers and ranked the third most common cancer among Malaysian women. Notably, the lifetime risk of acquiring cervical cancer is 1 in 144 and is greatest among the Chinese population.
How Is Cervical Cancer Preventable?
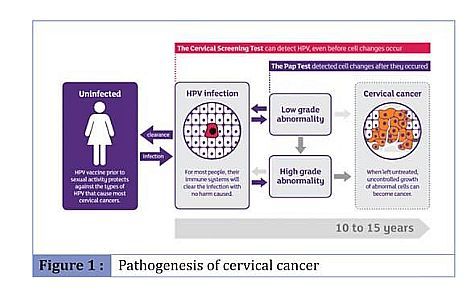
Almost all cases of cervical cancers are caused by a sexually acquired virus called the human papillomavirus (HPV), particularly, the high risk types 16 and 18. That said, HPV infections are extremely common and many of the other HPV types do not lead to cervical cancer. 90 per cent of HPV infections are cleared by our immune system within two years.
Persistent infection with high risk HPV can result in precancerous and cancerous changes in the cervix. There are some other factors associated with increased risk of persistent infection, namely, high risk types of HPV (types 16 and 18), weakened immune system (HIV, transplant patients and immunosuppressants), smoking, coinfections, number of babies born and young age at first birth.
However, the biggest risk factor for cervical cancer is not having had cervical screening.
Typically, it takes 15 to 20 years for cervical cancer to develop in a woman with a normal immune system. This allows time for early lesions to be detected through screening.
Imperatively, early lesions and HPV infections detected are often treatable.
In other words, cervical screening allows for early detection and treatment to prevent the development of cervical cancer.
Cervical Screening In Malaysia
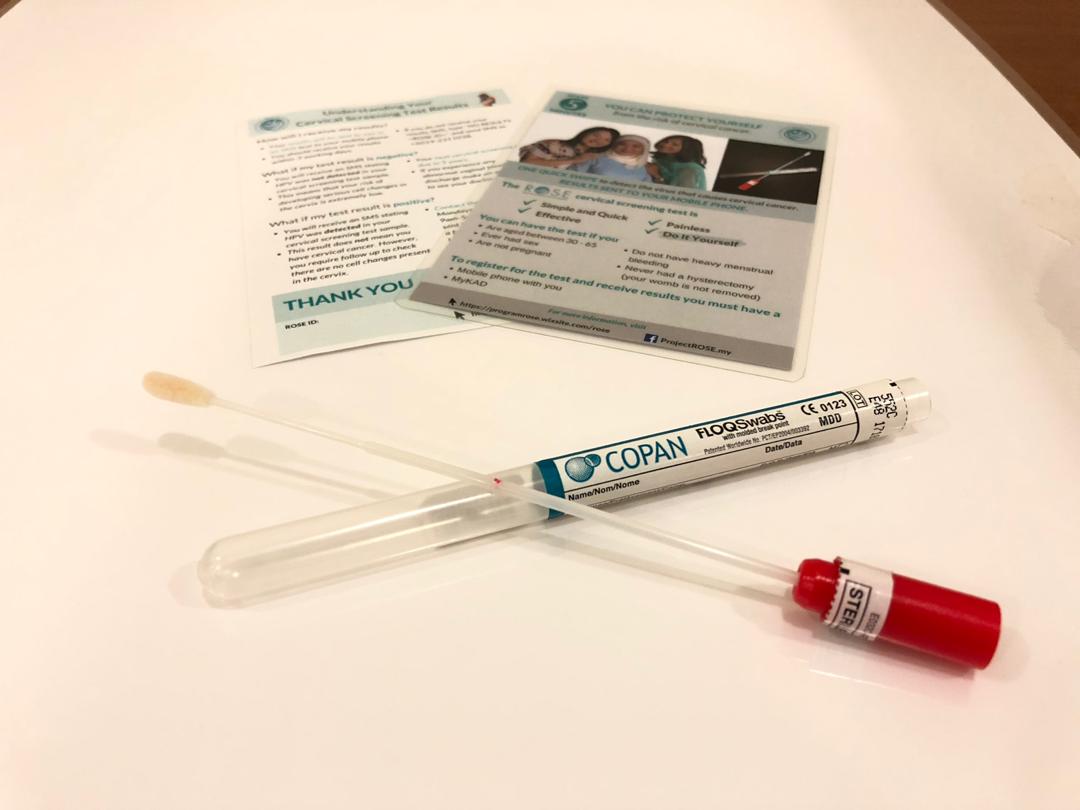
Currently, the screening tests utilised in Malaysia are mainly pap smear or/and HPV test.
| Pap smear | HPV test | |
| What is it? | A test that detects abnormal cells in the cervix | A test that detects presence of HPV |
| Sensitivity in detecting cervical cancer risk | Less sensitive | More sensitive |
| How is it done? | A sample is collected by a health care provider using a speculum and a sampling tool. The sample is analysed under a | Self-sampling by women themselves or by health care professionals using a self-sampling kit |
| microscope. | ||
| Who? | Sexually active women 30-65 years old *Sexually active women <30 years old are encouraged to screen | Sexually active women 30-49 years old (Ministry of Health Guidelines) *Women 21-29 and 50-65 are advised for pap smear screening |
| Screening interval | Yearly for two years. Continue three yearly if results were normal | Every five years |
| Where? | Government clinics & hospitals Private clinics & hospitals National population and family development board (LPPKN) ROSE Foundation National Cancer Society of Malaysia |
A negative result would warrant routine screenings according to the schedule given. A positive result would require further confirmatory testing and referral for appropriate treatment if necessary.
How Can We Play Our Part?
In conjunction with WHO’s Global Strategy to accelerate the elimination of cervical cancer, all countries must reach an incidence rate of less than four cases per 100,000 women. As previously mentioned, every country must reach this 90-70-90 global goal by 2030.
This involves collective efforts from various stakeholders. Medical students and organisations can raise awareness regarding cervical cancer by building knowledge around the disease, key prevention methods and early detection services.
For instance, Malaysian Medics International (MMI) has recently released a press statement on their call to accelerate the elimination of cervical cancer in November 2020.
Nonetheless, the road to the successful elimination of cervical cancer starts with women themselves. It is absolutely crucial for women of Malaysia to take matters into your own hands. Empower yourselves and others and prioritise your wellbeing. No woman should die from cervical cancer.
While many turn to doctors for screening and treatment, the difficulty is in taking the first step.