KUALA LUMPUR, Feb 28 – A national audit found imbalances in the number of hospital beds added to handle the surge of Covid-19 cases during the pandemic and nurses available to attend to patients, despite efforts to hire more nurses as temporary staff.
The Auditor-General’s (AG) 2021 Report tabled in Parliament last February 16 revealed that the filling of nurse positions is not equivalent to staffing requirements and does not follow the recommended level of care ratio, taking into account the scope of services provided at emergency and trauma departments (ETD).
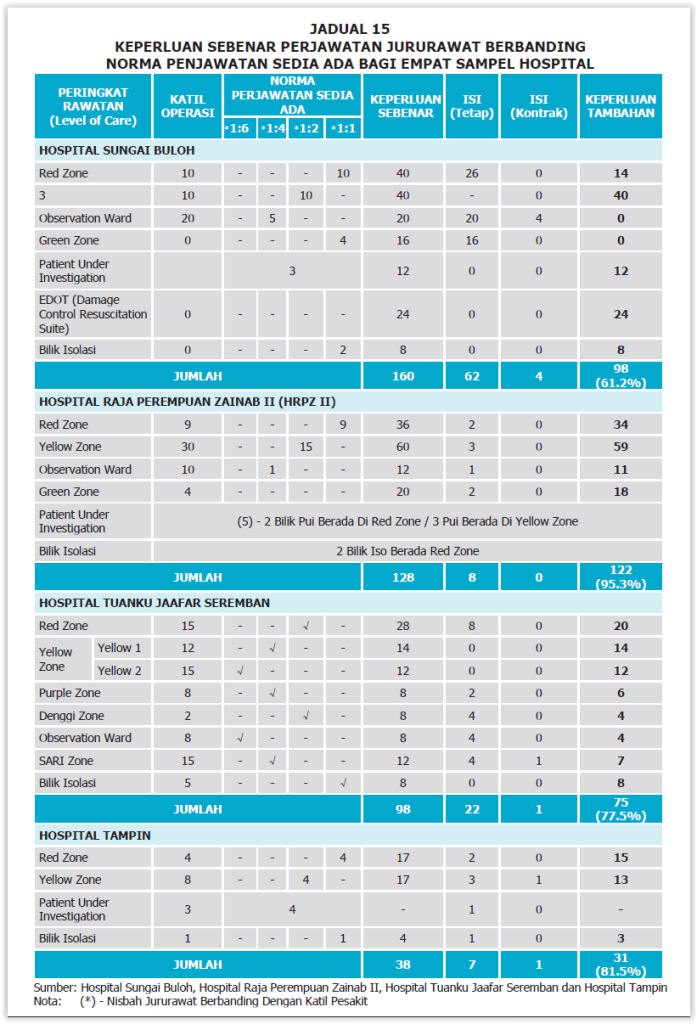
Audit checks found that the staffing at four government hospitals had a shortage of ETD nurses of between 61.2 and 95.3 per cent, with the availability of only seven to 62 nurses.
The four hospitals were Sungai Buloh Hospital in Selangor; Raja Permaisuri Zainab II Hospital (HRPZ II) in Kota Bharu, Kelantan; Tuanku Jaafar Hospital in Seremban, Negeri Sembilan; and Tampin Hospital, also in Negeri Sembilan.
HRPZ II had a shortage of 122 nurses in its ETD, Sungai Buloh Hospital (98 nurses), Tuanku Jaafar Hospital (75 nurses), and Tampin Hospital (31 nurses).
Additional nurses were needed across all levels of ETD care in all four hospitals, namely, the red zone, yellow zone, observation ward, green zone, patient under investigation, damage and resuscitation suite, and isolation room.
Using the same sample from the four hospitals, the audit also measured the number of nurses at intensive care unit (ICU) wards against the recommended level.
It found that the number of nurses placed in ICU wards during the Covid-19 pandemic was insufficient and had caused difficulties, especially when there were nurses on quarantine leave.
According to the AG report, all four hospitals increased their ICU bed capacity between 45 and 100 per cent, but the increase in nurses was only between 21 and 52 per cent.
The situation meant that the recommended nurse and patient ratio of between 1:1 and 2:3 in ICU wards were not met during the Covid-19 pandemic.
Based on audit estimates, the number of nursing shortages in ICU wards at all four hospitals during the pandemic period ranged from 44 (19.9 per cent) to 171 (43.7 per cent) nurses.
The shortage of nurses in ICU wards forced a shift in the level of patient care ratio to 3:4 in ICUs and changes to working hours from three shifts to two shifts, the audit noted. On average, each nurse had to work more than 12 hours per day and would be on double duty due to quarantine leaves.
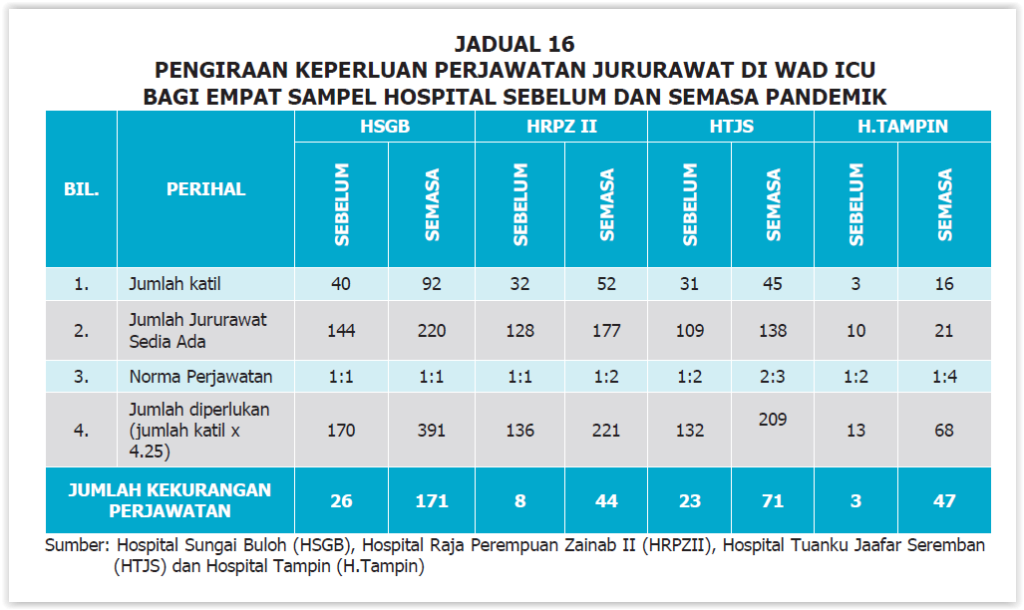
Hospital management had taken the effort to mobilise nurses from other general wards to the ICU ward. The mobilisation was only valid for the duration of the pandemic and the nurses involved would return to their original placement after the end of the period.
Despite the mobilisation effort, the nurse-to-patient in the ICU wards still could not be met as the mobilisation effort was limited to nurses trained in ICU care.
The audit concluded that the shortage of nurses according to level of care at ETDs and ICUs created a risky situation that caused patient care and treatment to be less ideal, in addition to repeated staff burnout in critical periods due to health worker shortages.
In a response by the Ministry of Health (MOH) to auditors last September 30, the government has approved MOH’s application for new permanent positions for the operations of new or upgraded facilities for 2021 and 2022; the numbers of the positions were not specified.
“To ensure the continuity of the health service, we forecast that 8,000 new positions for nurses are needed from 2023 to 2025.”








