KUALA LUMPUR, Feb 2 – A severe nursing shortage has led to suboptimal care in the neonatal intensive care unit (NICU) of a government hospital in Selangor, said a medical officer.
The government doctor revealed that in the acute (critically ill) section of the NICU of the Ministry of Health (MOH) facility where she previously served last year, one nurse attends to three babies, instead of the recommended one-to-one care – a problem that she claimed has been persisting for “so many years”.
The permanent medical officer is currently working in the paediatrics unit of a different MOH hospital in Selangor.
Additional issues that she raised are overcrowded emergency departments, shortages of housemen and junior doctors that affect patient care, bosses denying doctors leave, inadequate pay, and lack of sleep.
The medical officer was among the 1,652 respondents of CodeBlue’s poll among government health care workers last month that revealed 95 per cent believe Malaysia’s public health care system is currently in crisis, 98 per cent are angry at the situation, 73 per cent are thinking of quitting their job, and 52 per cent are willing to go on strike if one is organised.
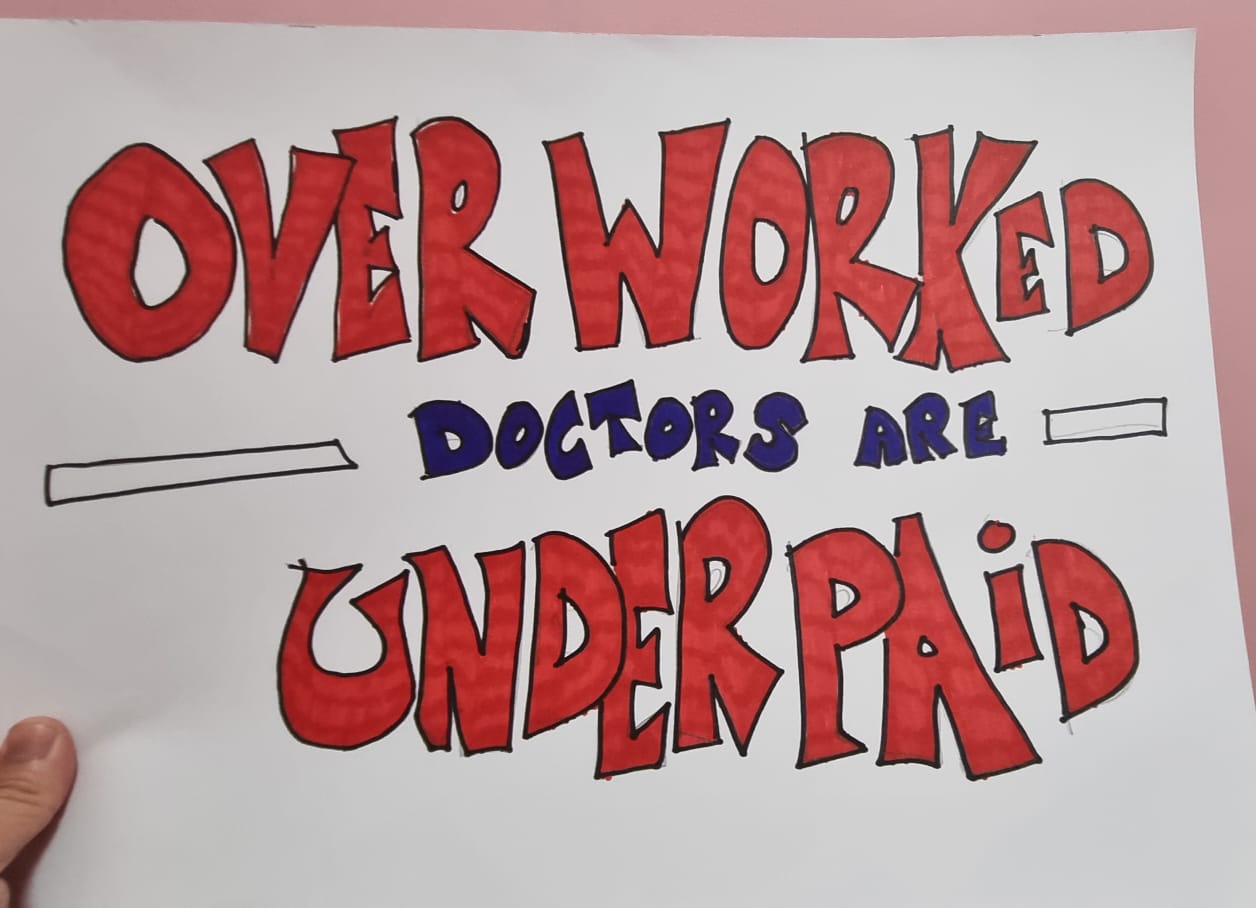
On workplace issues, 83 per cent perceive that the government isn’t serious in addressing issues in the public health care system, 80 per cent say they’re underpaid, 78 per cent complain of overwork, 74 per cent suffer from burnout, and 61 per cent feel insecure about their career progression. A quarter allege workplace bullying, while 2 per cent claim workplace sexual harassment.
Below is the medical officer’s story in her own words. As civil servants are prohibited from speaking publicly, CodeBlue is providing them anonymity. The transcript of CodeBlue’s interview with the medical officer has been edited lightly for clarity.
Suboptimal NICU Care Due to Nursing Shortage
I have no idea where all the nurses go. Whenever I speak to the nurses, I have friends who do nursing and stuff like that, they graduate and they don’t get a job in the government sector. I’m like, ‘Where are they going?’
Nursing shortage is always a problem. Ideally, when you have an ICU setting, you want to have one to one care: one nurse to one patient, or maximum one nurse to two patients.
When I was working in paediatrics in an MOH hospital in Selangor in 2022 (different hospital from the one I’m currently serving), the acute section of the neonatal ICU in my previous hospital had one nurse to three patients. It has been like this for so many years that it has become a norm.
In the neonatal ICU, there are four sections: one is acute, which are the critically ill patients. You have one nurse to three babies ratio.
Then you come to the intermediate area, where the patient is stepped down from the acute area. This is slightly better, but still not great, where it can go – one nurse to six patients.
And then you go to the stable area. The chronic patient area we have: area one, area two.
Area one is babies still on drip or probably some minor oxygen, or still in incubator just waiting for weight gain. So those kinds of babies, they can go up to 30 babies, where there’s just two nurses taking care.
And area two is usually mother and child. They’re very stable, waiting to go home so the mother rooms in with them. That’s just one nurse taking care of eight to nine babies.
Neonatal ICU is all babies less than one month old. It is definitely not very good care.
We have very small premature babies – the oxygen probe is supposed to be attached to them all the time in case if they have a reduction in oxygen or heart rate, then it starts to beep. Because they’re very premature, the part of the brain that controls their breathing is also premature. Anytime they can stop breathing, so they always have this monitor on.
There are many times when the monitor has gone off, but my nurses can’t cope to notice that. They are taking care of so many babies.
Medical officer, MOH hospital, Selangor
A coincidence — someone passing by, or after a while they realise and attend to the baby — but thank God nothing happened to the child. But of course, if you want to wait for something to happen, then it doesn’t look nice.
Mainly, I would say, increase the ratio of nurse-to-patient care. Also, there are not many paediatric ICUs around.
There’s a proper paediatric ICU only in Kuala Lumpur Hospital (HKL), PPUM (University Malaya Medical Centre), PPUKM (Hospital Canselor Tuanku Muhriz), HTAR (Tengku Ampuan Rahimah Klang Hospital), and a small one in Selayang Hospital. That’s about it.
When you have very ill children, sometimes some hospitals are regulating these children in their adult ICU. That is suboptimal care because it is shared with adult patients.
Medical officer, MOH hospital, Selangor
Adults have different kinds of bugs, and children have different kinds of bugs. When you have a shared space like that, children tend to get adult bugs which makes them more ill. That’s one thing.
It also affects the children’s mental health. Sometimes you have an intubated patient, like a very ill patient. That means that basically a tube goes through their mouth. They’re ventilated there. Somebody CPRing the patient next to you.
The young children don’t understand what’s going on. I’m sure it affects them. It’s very sad.
Someone older or a teenager, they just turn away. They know, ‘Okay, something’s not right.’ But younger children, they go, “Oh my god, what the hell’s happening?”.
If it’s a five- or six-year-old, they will have a lot of questions: “Mommy, what’s happening? Why are they doing that?”. Then you have to talk to them about death and this and that. “Oh, is my grandma also going to die like that one day?”.
Medical officer, MOH hospital, Selangor
So when they associate death with that kind of thing, CPR going on…
Of course, the lack of manpower is the main thing at every level. Equipment wise, it depends on the hospital. I think my hospital is fairly well equipped so I don’t have a problem with that.
Manpower. It comes down to manpower.
NICU Doctors Juggle Patient Reviews, Labour Room, and Emergency Caesareans All at Once
For paediatrics, we cover three areas. One person will be on-call in the neonatal ICU, one person is on-call in the emergency unit, and one person is on-call in the general ward — general ward is more-than-one-month-old babies up to 12-year-old children. All have different job scopes.
So the neonatal ICU, basically, as I said, there are four areas. The stable patients in the back areas – area one and area two – the step-down areas are usually seen in the morning by the night-before doctor, we call them post-call doctor. They see patients in the morning, then they give the plan, and then they leave.
The patients, on that day or on a weekend, are seen by the on-call person, and they see all the ill ones in front.
So after you review the patient, if you need to do any blood-taking, if you need to do any procedure to settle, and this may take up, depending on how many patients you have, you stay even up to 2.00pm.
And in between, you’re attending to four patients in the labour room. Any babies born, we have certain criteria, like maybe leaking of amniotic fluid from the mother. If leaking for more than 18 hours, the baby has a risk of infection, so the baby will be treated with intravenous antibiotics.
So all these patients are also attended by the same doctor.
And on top of that, if there is a delivery in the operation theatre (OT), like an emergency caesar, means there is something wrong with the baby that’s why they need to bring the baby out early, all these emergency caesars, we need to stand by. We are the same person attending there as well.
While you are reviewing patients in the NICU, you have to run to the labour room and OT – you have to juggle all that.
Some areas, like big centres, have many patients, so they may have two or more, depending on their centre. The present, because we have no housemen, basically like no other doctor to help, we only have two MOs to run the show.
Medical Officers Have Double the Workload Because of Housemen Shortage
From what I have surveyed around in hospitals, in Selangor especially, they are lacking in housemen, junior doctors.
Every level of doctors – like house officer, medical officer, or specialist – there is a lack. Every one of us plays an important role in the hospital service. So, even though they are trainee doctors (doctors in training), they actually have a small role that helps out with patient care.
When there is a lack, it does affect patient care. So that is one of the main concerns.
Medical officer, MOH hospital, Selangor
I’m not sure why, but most of the hospitals that I’ve asked around in Selangor, they lack housemen. There is a lack of housemen, so the medical officer (MO) has to do the houseman’s job as well. So it is double their job.
Housemen, of course, they are trainee doctors, so they have supervised blood-taking, keying in loads. If you have an IT-based system hospital, you have to order all the bloods or the X-rays and things like that.
It may look very minute, but when the MO takes over everything, it burdens them a bit. The MO job scope is mainly patient review, giving a plan, and carrying out certain orders, like referrals to other departments.
If there is difficult blood-taking or certain types of procedure that are more MO and senior doctor based, they will take over. Other than that, they also key in notes about patients and putting in entries.
If No Beds, No Choice – Patients Will Be Stranded in ED
It happens everywhere over time. You have a patient overload. It’s more apparent after the Covid pandemic. I’m not sure why, maybe because of the economic fall or anything like that, so there are more people coming towards the government sector.
What I noticed is that there are definitely days when we have no beds, so we try to maximise as much as we can. Eventually, patients are stranded in ED (emergency department).
In some big hospital centres, they have an observation ward in the ED, so patients are stranded there. There are bathrooms shared by many people. Nothing like a ward setting.
So it’s not exactly great for monitoring either, because ED is generally very busy. If no beds, no choice – they will be stranded in the ED overnight until the next day when we can discharge the patients.
When patients go home, only then can we take patients from ED to the ward.
RM200 Pay for More Than 24 Hours’ Work
And, of course, there is no pay revision.
I don’t know how many years there’s been no pay revision of our on-call claims, in god knows how long? We are still paid very minimally for being on-call overnight. And some hospital doctors work up till the next day — 5.00pm. So, I clock in today at eight in the morning and I leave the next day at five in the evening.
Some hospitals give us the next day, half day. So I clock in today at eight, next day probably I finish my morning rounds, so I can leave at 12pm.
And guess how much I’m paid for that? RM200.
The worst is when I work on a Saturday. I’m there the whole day. On weekdays, at least eight to five and my whole team is there so we do things together. On weekends, I’m a one-person, one-man show.
At the hospital I’m currently working at, I work the whole day — 24 hours — and the next day, I help with rounds as well, up to at least 10 to 11am; I get RM220. Just an extra RM20 for 24 hours of work compared to weekdays for about 16 hours of work.
In some busy centres with a lack of MOs, we are doing six to eight calls in a month. So it’s very, very tiring. It is very tiring.
There are ‘Good Days’ When You Get to Sleep for Five Hours
Then we go to the ward setting. In my centre, we have two and a half wards. One main ward can cater up to 30 patients. The other one is about 24. The other half-ward is a shared ward with a different department because they are dental, and they don’t really have many patients so we take half of their ward. They have about 16 beds there.
All the reviews of all these patients are done by two doctors on that day. We review the patient. These are patients with parents, so we have to talk to parents. We ask them how they are, check out their feeding, their oxygen levels, then examine them.
Then we have to key in the notes. If they are worsening, we need to do something for them that will take a longer time. If they’re well, they can go home then we need to do their discharge or their medications and give a plan for their upcoming follow-ups if they require those kinds of things.
Emergency have their own doctors. They will see the patients first, like a paediatric patient, and if they think, “Okay, this child I think needs further evaluation by paediatrics”, then they will call the doctor who’s in charge there.
Basically, all the patients that need to go to our ward will be screened by this doctor. They will look through. Anything they can discharge, they can do something for them, they will do, get it done, and discharge them. If they can’t, they will advise for admission. That’s how the patients come up to the ward.
This is the flow for medical officers. And on a weekend, there’s only one specialist who’s covering all these three areas.
The specialist’s job – they’re not going to come down to take your blood and all those kinds of things. Those are all done by the medical officer. The specialist’s main expertise is to give a good plan and management for the child, but all the plan and management is carried out by the medical officer and the houseman, technically.
But there are not enough housemen in most of the hospitals, so everything is done by the medical officer. They are very, very overworked.
Medical officer, MOH hospital, Selangor
Medical officers are all those doctors who are training to become specialists. They are studying. At the same time, they have a family to juggle, and then they also have to do on-calls.
You know, it takes me two days to recover from one on-call. Yeah, you can say your doctors have the on-call room, they have their own bathroom, but we’re barely there. We’re never there.
If you get one, two hours of sleep, it’s good enough. There are good days where you get to sleep for five hours, and that’s really good uninterrupted sleep.
Medical officer, MOH hospital, Selangor
But most of the time you have to attend to your patients. You have incoming new cases, everything.
If you compare it to overseas, they all work each shift. I don’t know what the timings are like, but in a day, it’s broken into three shifts or two shifts, so that is a lot more better. But of course, you need more doctors to do that.
In Malaysia, the Ministry of Health has always focused so much on house officers: house officers are being scolded, are being bullied, this, that, blah, blah, blah; but nobody bothered about the medical officer and the specialist. We all work a lot more than the house officers.
Over the years, I have seen so much changes done for the house officers. Now, they do shifts. They have a maximum of a certain amount of hours in a week that they can work. If you go beyond those hours, you have to give them leave and blah, blah, blah.
Everything’s so monitored, but nobody bothers about the medical officer.
Medical officer, MOH hospital, Selangor
Like I said, sometimes there’s only one specialist in a day doing on-call. If the specialist is not there or busy, it’s the MO who is doing the specialist’s job as well, because when a patient is dying right in front of you, you cannot wait for someone to come to give you orders.
The MO will have to buck up and do something while waiting for the specialist to come. You’ll be stuck there with one patient, and all your backlog of other work, you have to go back and settle that as well.
I’m in a permanent post. I’m not sure about the contract post, but I believe they’re paid a lot less than the permanent post. Because of that, a lot of young junior doctors are leaving.
A lot of junior doctors, because they’re in contract, get slightly lower pay, and they don’t see a future in career progression, unlike the permanent post. So a lot of them leave to the private sector and maybe open a clinic.
Also, my friends just informed me that another three medical officers are due to leave the department this month. They are really suffering there.
These three officers are seniors and have been doing the UK Masters paper, and they are in the final stages of their exams, and yet, they decided to leave because of no work-life balance.
My current hospital is a fairly new hospital, so patient load is just starting to increase. I feel that soon, we will be facing the same issues of lack of staff.
Paediatrics ‘Not A Favourite’, Manpower Really Affected
Towards the end of last year, I think from mid-June, every month, someone (junior doctors) left the department. And there was one month, up to four, five people leaving the department. That really affects us manpower-wise.
Paediatrics, generally, is not a favourite. Most of them who’ve been there very long eventually end up specialising.
You will have that mixture of some very seniors waiting to finish exams, some in the middle, trying to complete their overseas papers and trying to juggle work, and we have some very new (doctors) and juniors still thinking, “Should I still be here or should I jump to some other department?”.
Basically, we have a rule that once you’re in that department, you just have to give your best.
Medical officer, MOH hospital, Selangor
You have learning sessions, and teaching sessions for the junior MOs and the seniors who guide the juniors. They have a period of time, we call it tagging, where they learn. They’re given time to shadow someone senior and learn before they can be independently put on-call and things like that. It’s a very guided kind of thing.
It’s just that if you are in that department, you just have to buck up and do the job.
It’s very unfortunate. Some of them don’t want paediatrics, but because in a hospital, they only have a certain amount of posts for each department — so let’s say paediatric is maximum 20 slots, but now there’s a lot of empty slots there.
You want to go to surgery, but surgery is full so they get into paediatrics. They do it for a while, like six months or one year, until there’s a post in the surgical department that they like, then they move over if they want. That’s the trend.
Bosses Use ‘Service’ As A Reason to Deny Doctors Leave
I wouldn’t mind going on a strike. Seriously.
I just want some kind of improvement. We work so hard, but we feel unappreciated.
I think a lot of people resonate with the saying, “Service comes first”. This is something that you will hear very frequently in a government setting hospital where [if] you want to go for exams, you want to take a day for that exam, or some exams are overseas papers so you have to take a day off from work, or maybe you want take some time off to prepare for your exams on your own because every day at work.
So, it’s tiring.
Sometimes I just want to take some days to just study at home and things like that, and if there are not enough people at work, this is what the boss will say: “Service comes first”. If you need to let go of your off days, if you need to study less for your exams, so be it. Your service has to come first.
But you don’t understand that eventually, we better ourselves to provide a better service. So how can we provide better service if we are not keeping up with it?
But I also understand there is a lack of manpower. Government hospitals are always bursting with patients.
But that is the thing, I cannot find a balance. I can’t find a balance.
Medical officer, MOH hospital, Selangor
At least on days when we are not so busy, they could give some kind of leeway or something to help those who are studying for exams, to motivate them because they have a local masters’ programme.
Local master’s programme, those who are enrolled for it, have their own teaching time.
The professors will take them for teaching. They’re exempted from ward work during those periods and things like that, but it doesn’t happen in normal service government hospitals.
There are some who are probably not enrolled in those programs and sitting for overseas papers. They study in their own space, but there’s no one to guide them or anything like that.
Certain On-Call, Phone Bill Claims Denied
What’s worse, some HODs (head of department) don’t even allow us to make certain claims, not sure the reason. Examples of claims are:
Passive call claims. We have active and passive on-calls. Active means we are in the hospital and we can’t leave until the designated timing.
Passive is when we help cover our friends, as instructed by the HOD, usually on weekends, and this happened in all paediatrics in September. For example, Friday, I am on-call. I finish my call on Saturday at 8am, but I need to help cover some ward work, which usually ends at about 10am or 12pm, depending on the patient load.
According to MOH guidelines, I can claim for passive on-call. If I work less than four hours, it’s RM90, and if I work more than four hours, it’s RM150.
This, however, needs HOD approval; some HODs don’t allow us to claim.
Phone bill claims. Grade U54 onwards can claim for monthly phone bills of up to RM200, but some HODs don’t approve.
That’s how I feel, maybe some people don’t feel appreciated. And of course, the contract doctors definitely don’t feel appreciated because you work day in, day out, but you don’t get a promotion, you don’t get the same pay agreement as your other colleagues who have permanent posts. But you’re doing the same job.
Unhappy Patients Should Complain, So That Management Can Improve Things
Patients who walk in may also contribute to that feeling of being underappreciated.
I don’t expect anything from the patient. I don’t even expect a thank you because it’s my job.
Working in the paediatric department, just seeing the child recover and have a smile – it’s more than enough.
Medical officer, MOH hospital, Selangor
We have a lot of shortfalls. I’m not saying we are perfect because of the situation we are in. We are overloaded sometimes.
Patients wait so long. Imagine waiting with a child in the emergency department, which is like a dormitory with so many beds there, and you have to share a toilet, and then your child’s crying away. Then you have to shush them because next to you is probably an old auntie who is also waiting for a bed.
It is not easy. It’s definitely not easy when you have a sick child. So maybe there are shortcomings, a lot of shortfalls.
Sometimes I’m seeing so many patients that I cannot sit and console you, comfort you. So maybe they don’t feel like we are doing a great job. I understand from the patient’s point of view. We are not a private hospital; that’s the difference. We do what we can.
If they want to complain, they are unhappy, they should! They should, so then the management can look into this and do something to make it better.
Do Something. Change the System.
Do something about the contract doctor issue. Facilitate more people to be interested. Make sure you have a good team managing each hospital. Someone who’s capable. And, of course, the pay revision.
We can’t stop people from coming to the hospital, so patient overload will always happen. Try to change the system for doctors. Maybe change it to shift.
No, I’m not quitting.
Medical officer, MOH hospital, Selangor
I think most of the doctors that I know who left had resigned because they were contract doctors.Mainly because contract doctors felt like the private sector offered them something better.
Senior ones are all concentrated on finishing their master’s, completing their specialisation, and then leave for better pay.
The problem with more senior doctors is they just want to finish their master’s. They have this criteria called gazetting the specialist. There’s a certain amount of years you need to do work as a specialist, then only you can leave for the private sector.
So a lot of seniors are concentrating on that, and yes, a lot of them do leave later because of the pay issues. You definitely earn a lot more in private and probably not so stressful like working in the government setting.
The toxic culture in certain areas will be there, but I don’t think so in my work environment. I think the younger generation of doctors are now a lot kinder because they’ve also been through the whole thing with seniors.
So the younger generation are more kind towards their subordinates.