MONTREAL, August 8 – Dr Anthony Fauci, one of the world’s top virologists and director of the United States’ National Institute of Allergy and Infectious Diseases (NIAID), has called for a refocus on HIV/AIDS amid fears that progress in treating AIDS has stalled since Covid hit.
The Covid-19 pandemic undercut the HIV/AIDS response on all fronts, with HIV testing declining and prevention services – like harm reduction services for people who use drugs – facing disruptions in many countries, Dr Fauci said.
US Centers for Disease Control and Prevention (CDC) data showed a 17 per cent decline in HIV diagnoses in the US and dependent areas in 2020, down to 30,635 people, due in part to clinical care services disruptions and HIV test shortages during the Covid-19 pandemic.
Fewer HIV-positive people started antiretroviral therapy (ART) in 40 of 50 countries in 2020, while harm reduction services for people who use drugs were disrupted in two-thirds of 130 countries that same year, Dr Fauci said, citing the United Nations secretary-general’s report in May.
“We have got to get HIV/AIDS back on the forefront of the radar screen of the public health community at every single level, despite the fact that we are going through simultaneous outbreaks of a history pandemic with Covid and the emerging outbreak of monkeypox,” Dr Fauci said at the 24th International AIDS Conference (AIDS 2022) in Montreal, Canada, last July 31.
The HIV treatment gap remains wide globally, with 9.7 million people living with HIV still not on ART, despite data showing a dramatic decline in global AIDS deaths with increasing ART coverage over the past two decades. About 38.4 million people live with HIV as of last year.
Dr Fauci said that advancements in ART have also allowed many adults infected with HIV to have an “almost normal” lifespan.
In addition to getting people on treatment, treatment gaps also exist in adherence to ART – which is essential to suppress the viral load and achieve optimal HIV care.
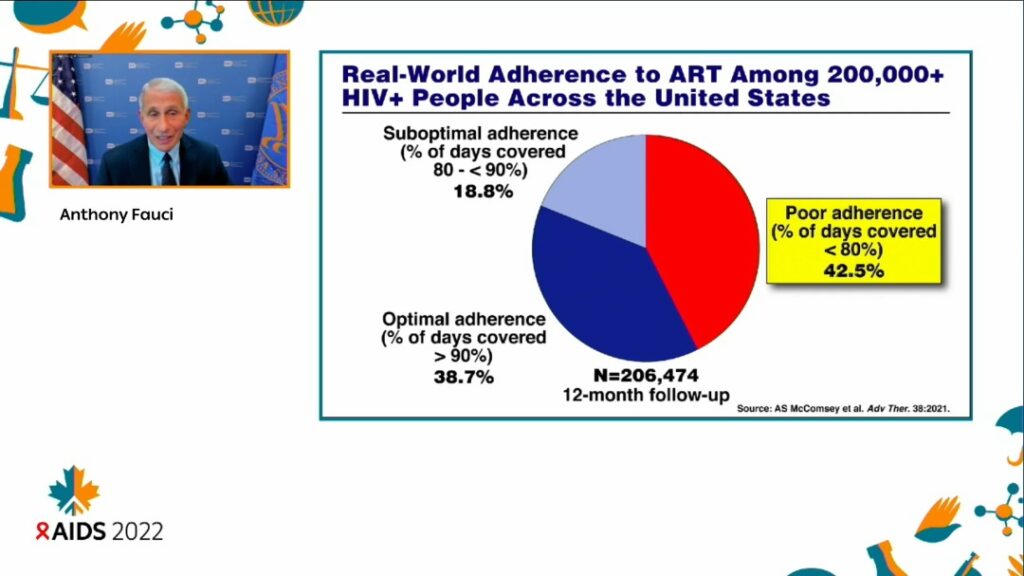
A study on real-world adherence to ART in over 206,000 HIV-positive people across the US showed that 42.5 per cent of participants had poor adherence to ART, Dr Fauci said.
“These are statistics from the US, but in many respects, there are variations of this throughout the world.
“If you look at the dark blue, in the lower left, the optimal adherence, namely the percentage of days covered is greater than 90 per cent, is less than 39 per cent. The people with suboptimal but reasonable adherence between 80 and less than 90 per cent, are seen at about less than 19 per cent.
“But look at the red slice of the pie for adherence where the percentage of days covered is less than 80 per cent. It is almost half of those in the US, a developed nation,” Dr Fauci said.
Apart from treatment, access to preventive tools such as pre-exposure prophylaxis (PrEP), a highly effective medicine that can reduce a person’s chance of getting HIV, remains uneven.
Truvada, one of the main brands for PreP, was the first drug approved by the US Food and Drug Authority (FDA) that lowers the risk of sexually acquired HIV infection. According to the CDC, PrEP reduces the risk of getting HIV from sex by 99 per cent and injection drug use by at least 74 per cent.
“So we know that as a fact. But getting back between the balance of implementation and discovery, the cumulative number of PrEP initiations, although it dramatically increased to around 2.8 million, is the good news.
“But the sobering and somewhat distressing news is that the global need is measured in tens of millions, much more than what we are doing,” Dr Fauci said, citing PrePWatch data.
U=U: Undetectable Equals Untransmittable

Earlier in the session, demonstrators from the U=U (‘Undetectable equals Untransmittable’) movement took centre stage in a rallying cry for more investment in people living with HIV.
“U=U”, a short phrase used by HIV researchers and advocates, is an affirmation of clinical evidence that people living with HIV, who respond to antiretroviral medication and achieve an “undetectable” viral load (the amount of HIV in the blood), cannot sexually transmit the virus to other people.
In other words, ART is HIV treatment that is also prevention.
“We are tired of your excuses. We are tired of your bullshit. We know, as people living with HIV, that we are the greatest tool to end HIV. Today we are calling on governments, policymakers and donors to invest in people living with HIV,” said Michael Ighodaro, a Nigerian activist and an advocate for LGBTQ rights and HIV prevention.
“We know that when you invest in us, we can achieve U=U, and when we achieve U=U, there will be a drastic reduction of new infections, and that means we can end HIV.
“This is not just a personal benefit to us. It’s a public health benefit, it’s an economic benefit. Invest in people living with HIV and end HIV today,” Ighodaro said.
Global efforts to address HIV in 2022 and beyond should not only cover implementation gaps, such as access to testing and PrEP, as well as adherence to ART, Dr Fauci said, but also the development and delivery of improved treatment and prevention interventions.
He cited recent progress made in developing long-acting ART that allows HIV medication to be consumed over longer intervals instead of daily and ongoing studies about using broadly neutralising antibodies (bNAb) against HIV.
“To me, it is unconscionable for us now – because we are dealing with so many other challenges – to slow down anything we’re doing with HIV. In fact, we need to accelerate what we’re doing with HIV,” Dr Fauci said.
“Dealing simultaneously, as I do every day, with Covid, monkeypox and HIV, we can do all three at the same time. This idea about one competing with the other is understandable, but not acceptable. We’ve got to put all our forces on all three at the same time.”
He added: “Remember that this (HIV/AIDS) is a 40-year pandemic, and this can’t be a timeout. You don’t call a timeout on a pandemic and say, ‘come back next year’.
“You’ve got to continue with all your might to continue to address it, and that’s what, one of the things that saddens me is when supply chains stopped, when testing stopped, when tuberculosis (TB) work stopped – that was something that was really painful.
“We’ve got to get back on track.”








