The Seventh Malaysia Plan (1996-2000) promised a new district hospital in Lawas. Kam Agong was then pregnant with her eighth child in 2002. She was only 44 years old and otherwise in good health. But she died from excessive bleeding after delivering her child.
Twenty years after her death, the hospital remains an unfulfilled promise. High-risk pregnant women still need to undertake long arduous journeys to either Miri or Kota Kinabalu for specialist care and caesarean sections.
Reforms of the health care system are long overdue and urgent. There have been 14 studies since 1985, with near-unanimous consensus, and yet, reforms were amiss.
What Are The Challenges To The Health Care System?
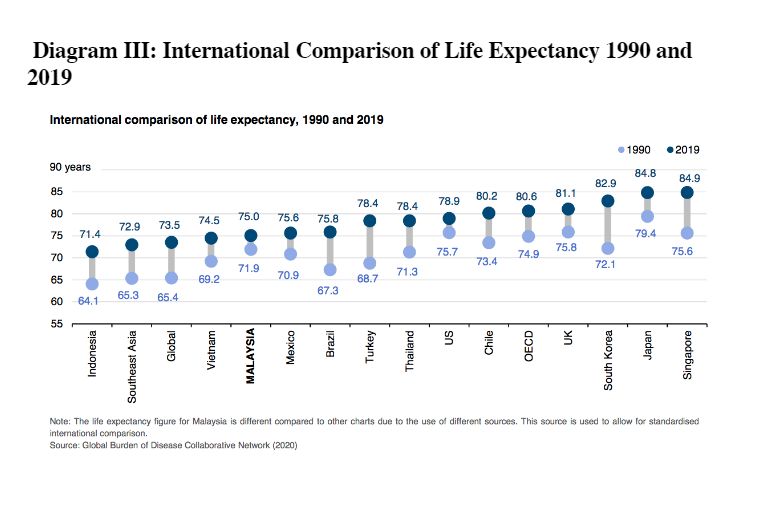
Our past leaders have bequeathed us with a health care system which performed beyond expectations, and was respected globally. In the previous century, deaths of pregnant women, infants, and children was relatively low, given Malaysia’s economic status, compared to countries at a similar economic development.
However, improvements in such critical indicators in the 21stcentury have stagnated. Deaths among pregnant women, infants, and children made no discernible progress for the last two decades since 2000.
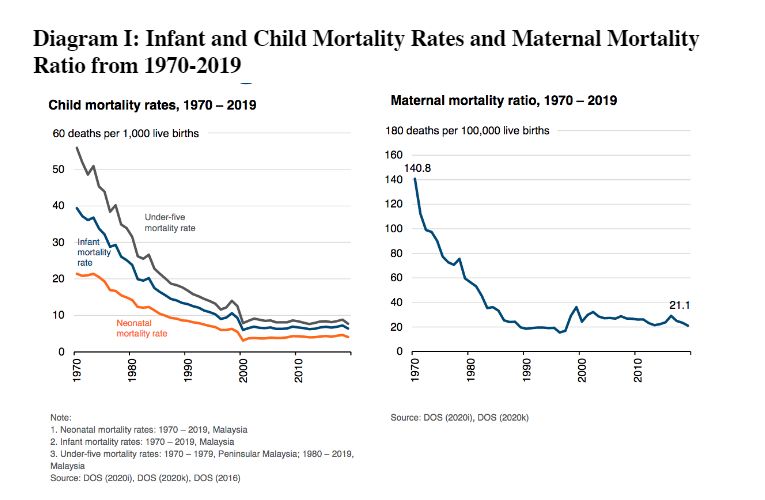
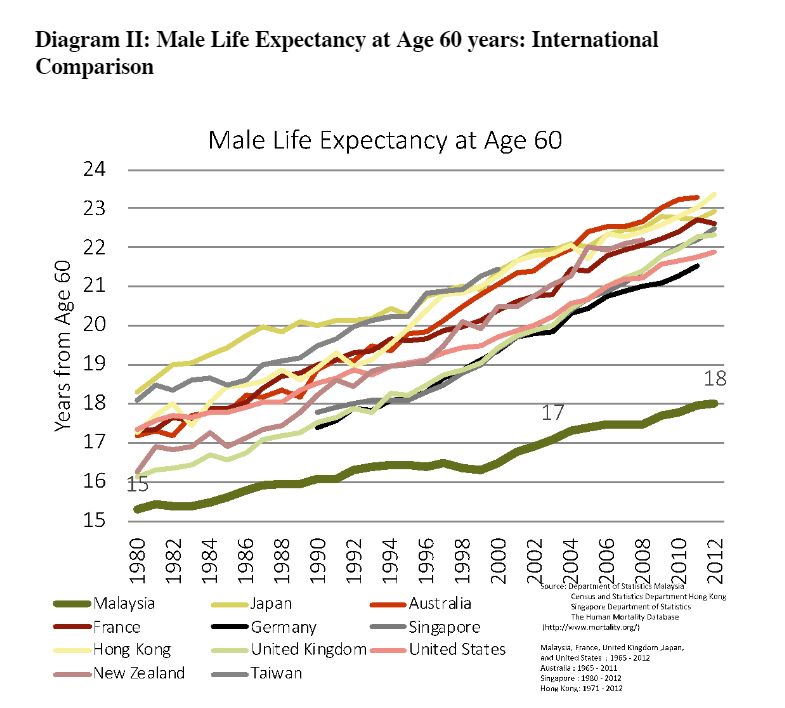
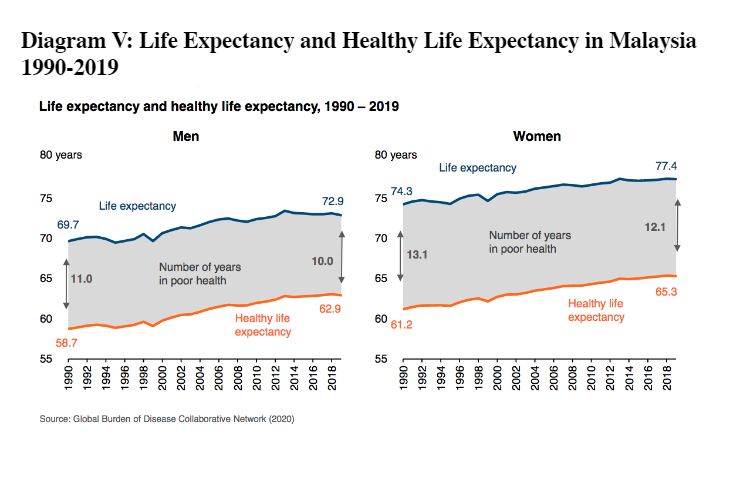
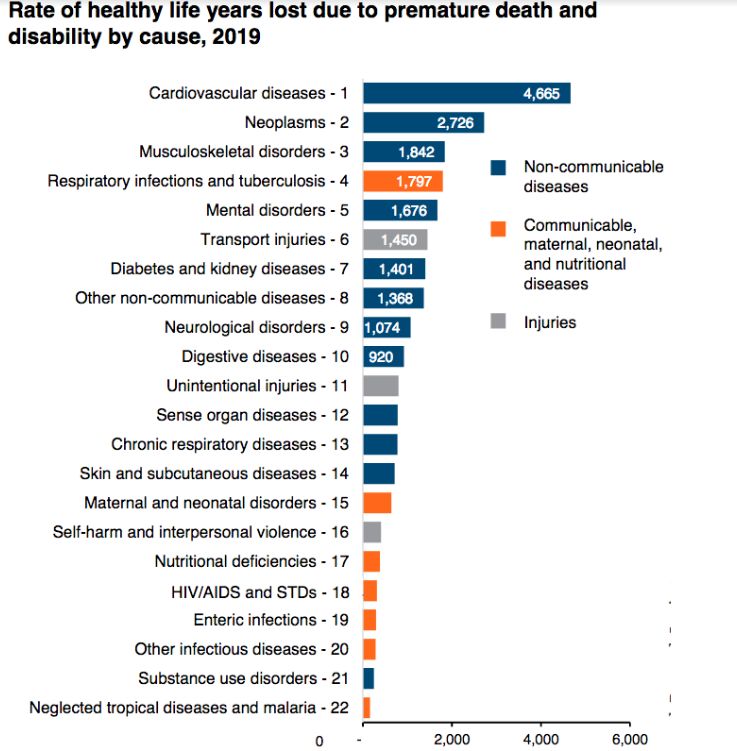
Similarly, although life expectancy has been improving, the pace of improvement among males who have reached the age of 60 — a proxy for non-communicable diseases (NCDs) — is glacial, compared with comparator countries, leading to a noticeable gap.
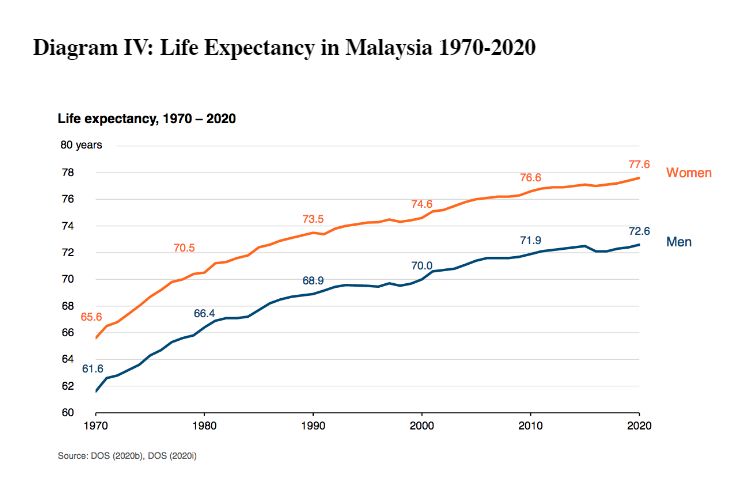
There were only 11 years (male) and 12 years (female) of gain in life expectancy over a 50-year period from 1970 to 2020.
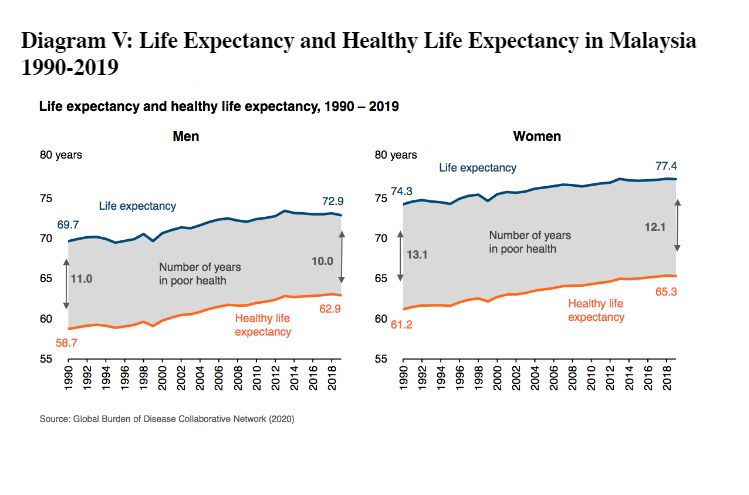
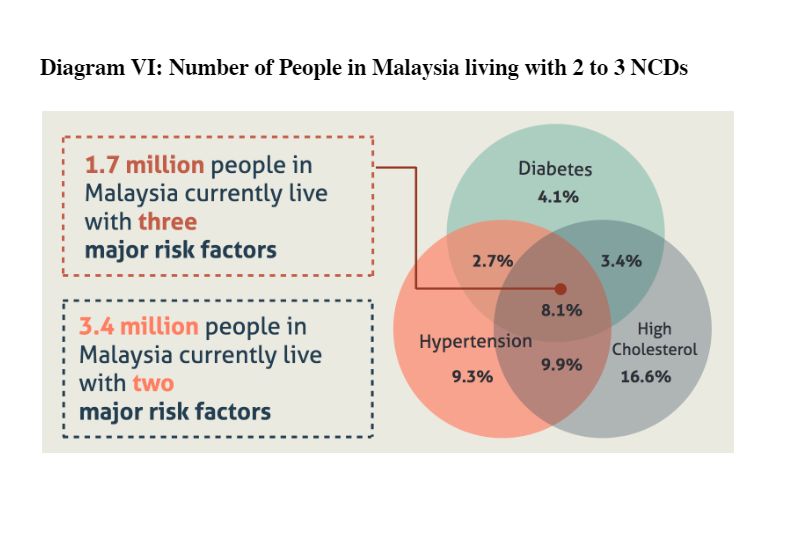
Furthermore, although Malaysians are living longer, they are not spending those extra years in good health. According to the 2019 National Health and Morbidity Survey, 1.7 million (8.1 per cent) live with three NCDs, and 3.4 million with two NCDs. 73.6 per cent of total health loss was due to NCDs.
Inequalities in health are rife. The Khazanah Research Institute (KRI) has reported wide inequalities. Life expectancy is shorter in states with lower incomes.
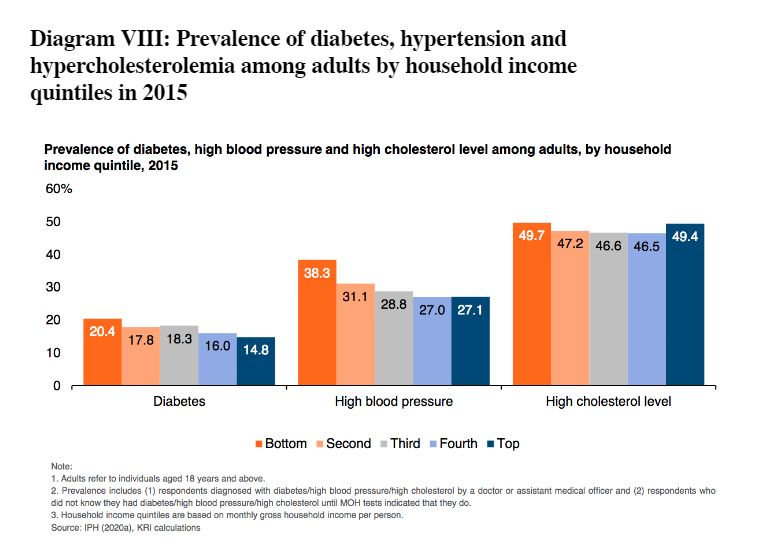
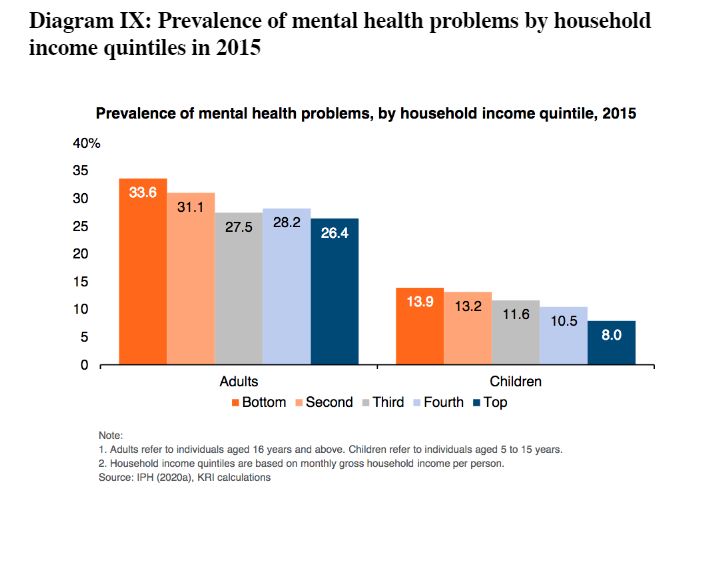
Diabetes, hypertension, and hypercholesterolemia are more prevalent in lower-income groups. Mental health problems are more common in lower income families.
Such data provide the evidence that the tragic stories such as Kam Agong are not mere anecdotes, but a systemic problem for Malaysia.
Much has been written to highlight the everyday experiences of ordinary Malaysians faced with inadequate public investment in health. The Auditor General in 2018 reported that public hospitals are understaffed, overcrowded, and underfunded.
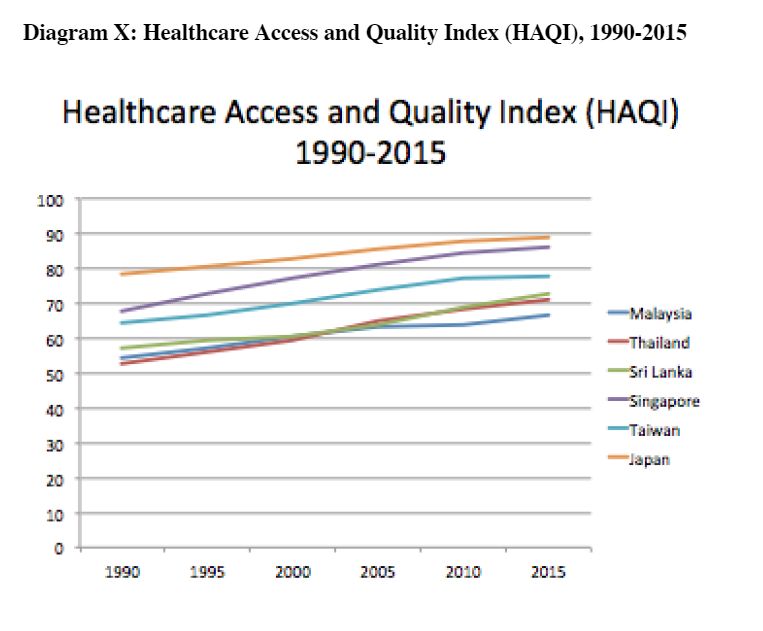
Much praise has been heaped on our health care services, especially hospitals which service expatriates and high-income individuals, but the reality for the masses is that we are only ranked 84th on the Healthcare Access and Quality (HAQ) Index.
The HAQ Index measures a person’s access to quality health care that would protect that person from amendable mortalities due to 32 different diseases.
And as Diagram X illustrates, we are well behind our neighbors, Sri Lanka, Thailand, Singapore, Taiwan and Japan on the HAQ Index for the years 1990-2015.
Key Determinants Of The Transformation Of Our Nation’s Health
As alluded to by KRI researchers as recently as April 2022, there is extensive evidence to show that societal factors such as education, housing, welfare, environment. and occupation have a much greater impact on nurturing the public’s long-term health.
Often described as the social determinants of health, social, economical, commercial, environmental and educational conditions are undoubtedly the most powerful influencers of the people’s health.
Inasmuch as the reforms by the Ministry of Health (MOH) are overdue, it is not the be-all and end-all of the state of the nation’s health.
We would be missing the forest from the trees if the nation is yet again led to think that a better and reformed MOH would transform the people’s health. The nation faces multiple challenges to reduce health inequalities and improve the people’s health.
It is obvious from the KRI report that one of the most powerful drivers of good health is the ability to secure an adequate income. The Covid-19 pandemic has further amplified this problem.
The number of families and children experiencing poverty has increased from a poverty rate of 5.6 per cent in 2019, to at least to 8.4 per cent of all households in 2020, due to the pandemic.
We are very hopeful that the White Paper will reframe the national health agenda. The people’s health needs to be valued as an asset, and health aspects must be considered by the government across all its policies.
The government needs to drive policy decisions which would create social, economical, commercial, environmental, and educational situations which contribute to healthy lives.
Apart from the reformation of the health care system, these wider and more powerful social determinants of health must be prioritised, and the inequalities in health addressed appropriately and urgently.
The social discriminants of health can only be successful if it is incorporated within the context of Health in All Policies (HiAP) of a whole-of-government approach.
The HiAP government philosophy considers seriously the health implications of all public policies across all sectors, and ensures that they synergise to enhance population and health equity, and also avoids harmful impacts on health.
One of the most difficult conundrums for a health reform agenda is the lack of, or failure of a multi-sectoral integration of agencies and relevant authorities.
As the MOH labours on about the seriousness of NCDs, to tackle this problem does not only involve reforms in health. Neighbourhoods and built environments also play a crucial role in enabling the practice of a healthy lifestyle.
We tell people to exercise, yet there are no safe paths within the vicinity of the community, no proper bicycle lanes, poor roadworks that support pedestrian and bicycle use, and poor facilities for hiking trails and nature reserves.
Stunting (low height for age) of our children below 5 years old has increased from 13.4 per cent in 2015 to 21.8 per cent in 2019. Short term effects of malnutrition includes impaired brain development, lower IQ, and a weakened immune system with recurrent infections, while in the long term it leads to shorter adults, greater risk of NCDs, lost productivity, and increased health care costs and premature deaths.
There are multiple compounding factors which needs to be addressed holistically, which go beyond the MOH reform agenda. This includes addressing the low-income status of families, alleviating poverty, better housing, better social security safety net, better health education, and food security, which are all social determinants of health.
The reformed health care system should invest better in preventative health care services (68 per cent of total health expenditure spent on curative care services in 2018), which would ensure good antenatal care, exclusive breastfeeding in the first six months of life, optimum complementary feeding in the first two years of life, and optimised family-based diets for 2 to 5-year-olds.
The collaboration and synergy of multiple ministries and agencies are essential to ensure success of nurturing the good health of our youngest and most vulnerable within the context of the HiAP government philosophy.
There are three major areas in the health care ecosystem that need to be reformed, namely transformation of the public health sector, regulatory reforms of the private health sector, and sustainable health care financing.

This new paradigm in health care is captured in the maxim “Technology-native, person-centered integrated care, based on value and choice, supported within a health empowering ecosystem”.
And as the dictum goes, health is wealth. Good health leads to the people’s wellbeing, enhances their productivity, and better contributes to the wellbeing and prosperity of the nation.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.





