KUALA LUMPUR, Nov 30 — Harm reduction, or interventions that aim to reduce the risk of HIV infection in Malaysia, can prevent thousands of new HIV cases and save millions of ringgit in annual direct health care costs.
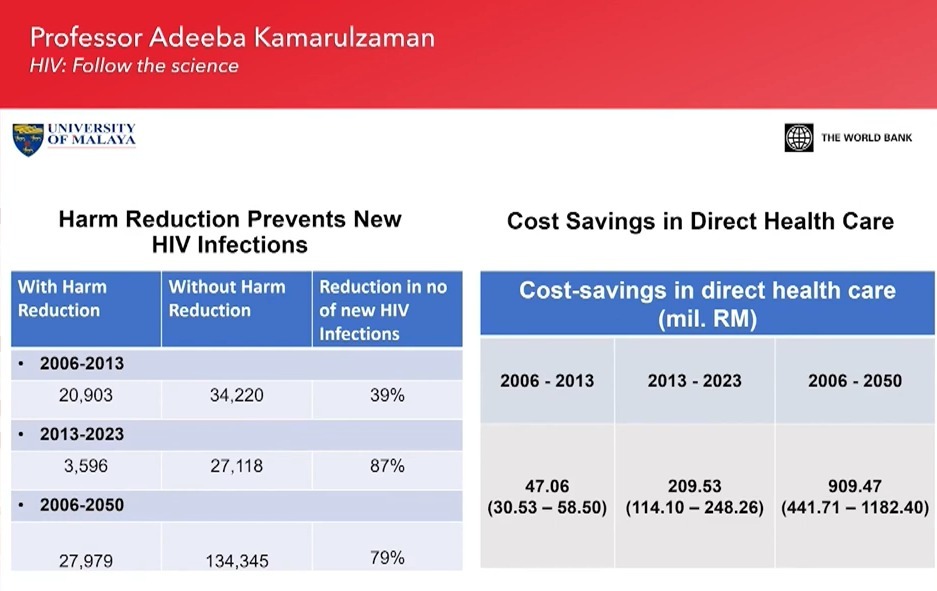
International AIDS Society president Prof Dr Adeeba Kamarulzaman, in her presentation at the Chinese Center for Disease Control and Prevention (CDC) and Centre for the AIDS Programme of Research in South Africa (CAPRISA) World AIDS Day 2021 webinar on Monday, showed that harm reduction prevented up to 39 per cent or 13,317 new HIV infections in Malaysia from 2006 to 2013.
At the same time, the estimated cost-savings in direct health care spending over the period for HIV were about RM47.06 million.
In another projection between 2013 and 2023, harm reduction programmes in Malaysia — which involve people who inject drugs (PWID) — were estimated to reduce new HIV infections by up to 87 per cent or 23,522 cases and RM209.53 million in health care costs.
Over a longer period from 2006 to 2050, Malaysia’s harm reduction programmes for HIV are projected to bring new HIV infections down by 79 per cent or 106,366 cases and direct health care expenditure by RM909.47 million.
“We have seen the world over that knowing your pandemic and following the science can give rise to great outcomes, whether it’s in Covid-19 or in HIV. In Ukraine, China, and Malaysia where we were witnessing increases in HIV incidence due to injecting drug use, the implementation of harm reduction resulted in the reversal of the pandemic in the three countries.
“The opposite would happen if these evidence-based intervention programmes are not implemented, as has been seen in the Philippines and in countries of the former Soviet Union. Following the science not only saves lives, but it also saves money,” Dr Adeeba said.
Malaysia’s harm reduction programme primarily consists of the Needle and Syringe Exchange Programme (NSEP) and Opioid Substitution Therapy (OST).
The NSEP is a programme where used needles and syringes are exchanged with sterile ones among intravenous drug users, while the OST or the Methadone Replacement Therapy (MRT) is when methadone — a drug that is similar to morphine in its effects but less sedative — is given to patients to reduce opioid dependence.
According to the Global Aids Monitoring 2020: Malaysia HIV/AIDS Progress Report, sharing injection paraphernalia or equipment has been the main mode of HIV transmission in Malaysia since the beginning of the HIV/AIDS epidemic in 1986.
However, in the past decade, the country observed gradual changes in the HIV epidemic landscape from predominantly PWID to sexual transmission. The proportion of sexual transmission for HIV infection increased to over 90 per cent in 2019.
Annual reported HIV infections hit a peak of 6,978 cases in 2002 but have since declined to 3,564 cases in 2019. In 2019, the estimated number of people living with HIV in Malaysia was about 87,000, with total AIDS-related deaths amounting to 2,685.
Dr Adeeba said in order to bring an end to HIV/AIDS, continued investment in new tools, as well as research and development of HIV, are needed. She said investment in HIV cure research plateaued between 2018 and 2020 at US$323.9 million to US$337.4 million, compared to a steep increase in funding in the years prior from US$104.7 million in 2013 to US$323.9 million in 2018.
“Certainly, we must continue to invest in cure research, but a little worrying is that we have seen a plateauing in funding related to this research programme.
“As you can see, HIV science has remained active despite the attention that rightly so has been given to Covid-19 research, and we must continue to find new ways to implement the tools that we already have, from like I mentioned, syringe programme and opiate agonist treatment that needs to be scaled up.
“But we also have a not so new tool in the form of pre-exposure prophylaxis (PrEP) that is entering its second decade although the uptake of PrEP has been rather slow since the clinical trials confirming the effectiveness of PrEP.
“Fortunately, in the last few years, we’ve seen more and more countries adopting this effective prevention tool. However, I think it remains to be seen, although adopted international policies, whether PrEP will be scaled up effectively to bring about a reduction in new HIV cases around the world,” Dr Adeeba said.
Commenting on equitable access to HIV/AIDS cure, Dr Adeeba said: “HIV has traditionally affected people at the margins and unfortunately, I think, in terms of government priorities in financial investment, especially with domestic funds, people who inject drugs, MSM (men who have sex with men), and sex workers or transgenders may not be high up on the priority list of government investment in health dollars.
“Hence, I think, despite us having all these tools at our disposal, we’re still struggling to get them to where it’s most needed. We’ve been living through this in the last two decades — we have great tools and yet it’s not going to many places to where it’s most needed because of all these inequities, underpinning this is, of course, stigma and discrimination, criminalisation of behaviours that have plagued the HIV response for many years.”