KUALA LUMPUR, July 20 — Minimising social interaction is the key measure individuals should take to avoid Covid-19 infection, besides getting vaccinated, improving ventilation, and maintaining personal fitness, Dr Amar-Singh HSS said.
The senior consultant paediatrician advised the public to strictly follow home safety bubbles — keeping contact only with members of one’s household — by adhering to all the Covid-19 standard operating procedures (SOPs) and embracing new norms.
He stressed that there is currently no “safe” number for people to gather, amid a surging epidemic despite over six weeks of a national lockdown.
“Keep a strong home safety bubble,” Dr Amar said in a recent virtual talk titled “Covid: The Current Situation in Malaysia and the Churches’ Response”, organised by the Methodist Church of Malaysia.
“If you see your neighbours when you’re jogging by the side of the road, you don’t stop and talk. I still see neighbours talking to each other every day. I’m worried for them as it is a very risky thing to do.
“Don’t interact with anybody. You want to talk to your neighbour, you give them a video call and talk to them.
“You want to buy food, you should buy from shops that give you an opportunity to buy from the outside if possible. Try not to walk into a shop, you can scan the QR code from the outside. All restaurants should actually consider moving services outdoors or offering takeaway at the entrance.”
He also called for a work safety bubble as well for those who go to their work stations.
“People who work together must be honest. I call it a trust bubble. You must tell everyone you work with the moment you have contact with who is positive, or if you’re infected. If you are unwell, you should not come to work.”
Besides that, Dr Amar advised the public not to eat lunch together with their work colleagues because unmasking in a group indoors will increase the risk of being exposed to the coronavirus. He also suggested not removing face coverings in the workplace, including places like toilets, due to poor ventilation.
Dr Amar said that the daily reported Covid-19 cases by the Ministry of Health (MOH) does not reflect the actual scenario, as the number of new infections depends on the number of Covid-19 tests.
“Reported numbers depend on testing, which, sadly, are not shared with the public,” said Dr Amar.
MOH shares cumulative Covid-19 tests done nationwide as of the day, instead of publishing daily test numbers. Testing data by state or district are also not made available.
“Don’t focus on the clusters, focus on the community spread, which is the bigger part of the pandemic,” said Dr Amar.
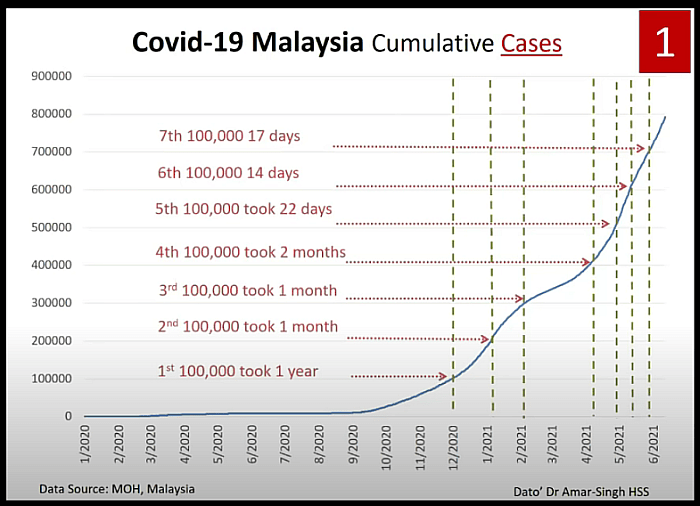
Malaysia reached its first 100,000 Covid-19 cases in 334 days on December 24 since the virus hit the country. But the next 100,000 reported cases took a month. The fifth 100,000 cases were accumulated in only 22 days, while the sixth and seventh 100,000 cases took 14 and 17 days respectively.
“So right now we’re moving up by 100,000, every 15 to 16, maybe sometimes 17 days, and recognise that this means that our pandemic is moving at a very fast rate right now in our country.”
Dr Amar also pointed out the high Covid-19 test positivity rate in Malaysia last month, ranging from 6.64 per cent to 7.68 per cent, which denotes more undetected cases in the community (it has since risen to 8 to 9 per cent). He mentioned that the Movement Control Order (MCO) only managed to reduce coronavirus cases for a short period of time.
“Our pandemic is growing, not coming down. So the MCO has halted it for a very short time and now it’s going back up again, mainly because it’s spreading in the community unchecked.”
Dr Amar highlighted that Malaysia’s mortality rates due to Covid-19 are rising, including death rates among non Covid-19 patients. He said that the full usage of intensive care unit (ICU) beds have led to insufficient beds for new critical patients and patients with other diseases, leading to the deaths of patients like critical accident victims, heart, and cancer patients.
“Our ICU beds are very full. We’ve now repurposed the general beds to use for ventilating people, which is not ideal. A portion of our ventilated patients in ICU are dependent. They’ve been there for a few months, some of them”.
“So that clogs up the whole ICUs from being used by people who get fresh Covdi-19 illness. So once this happens, mortality rates will go up.”
Dr Amar said that mortality among non-Covid-19 patients during the epidemic should be reported, especially those who cannot get an ICU bed.
Dr Amar also noted that ICU care requires trained health care personnel and mortality will rise with insufficient staff looking after ventilated patients. He claimed there are some Stage Four and Stage Five Covid-19 patients with severe disease who are still waiting to be admitted into hospitals nationwide; being ventilated in the emergency departments.
“If all my colleagues in the country could speak, maybe the horror of what they are facing might actually galvanise the public to actually be more careful about our situation,” he said.
“The first 500 Covid-19 deaths took us about a year. But right now we’re taking seven days to get 500 deaths. Five hundred people are dying from Covid-19 every seven days, and our mortality rate has gone up.”
“Previously 0.4 per cent of people who got ill died. Now it is 1.3 per cent. So that’s a big difference. We’re losing almost three times as many people as we did at the beginning of the pandemic.”
The maximum usage of ICU has also pushed doctors to triage patients based on their chance of survival, Dr Amar added.
“So this is very painful for doctors to do and we don’t like it. But you have to decide who you want to rescue. Most doctors will probably rescue the ones that can do better than the ones they think have a high mortality.”
Dr Amar also mentioned that the 1.3 per cent case fatality rate varies according to the age of the patients. “If you’re older, you’re more likely to die. If you’re younger, you’re less likely to die. In addition some who leave the ICU also die later — our crude estimate is that 10 per cent of those who leave ICU, die. In addition we don’t have any idea of the collateral deaths at all.”
From May 1 until July 14, Malaysia reported a total of 531 brought-in-dead Covid-19 cases. That is 10.6 per cent from the total Covid-19 fatalities recorded in the same period of time.
Dr Amar said that there is no data to identify the status of these people who died from Covid-19 before they could seek medical treatment. He said that they could be those who did not know they were positive and then they died at home, or those who tested positive and were asked to stay at home before getting a place in overwhelmed quarantine centres. Brought-in-dead cases could also be people with Covid-19 who developed critical illness in a shorter period of time.
“We don’t know any of this data; it is not available to us. But to lose 10 per cent of our deaths from brought in deaths suggests to us that the system has failed across the board and is no longer responsive to what is happening.”
Dr Amar also noted that “long Covid” is another issue that should be tackled in the epidemic. Although Malaysia does not have comprehensive data on long Covid patients, Dr Amar said that MOH data shows that 60 per cent of ventilated Covid-19 patients who were discharged from ICU are suffering persistent effects from coronavirus infection.
According to Dr Amar, since the end of June, almost 72 per cent of the small sample of Covid-19 cases with identified variants of concern in Malaysia were the Delta strain that originated from India and might be the dominant cause of the latest surge of Malaysia’s outbreak.
“Our problem is that there is very little genome testing in our country compared to other countries in our region.”
Besides that, Dr Amar also commended the ramping up of Covid-19 vaccination in the country, as he called for even faster inoculation rates.
“We’re not expecting the vaccines to stop all infections. We want the vaccine to prevent severe infection, or hospitalisation.”
As of July 18, a total of 41.9 per cent of the adult population in Malaysia has received the first dose of Covid-19 vaccine, including 19.4 per cent fully inoculated.
However, Dr Amar noted that the vaccination programme should be accelerated in parallel across all states because the Delta strain can easily increase Covid-19 infections in other states, as they start to ease movement restrictions.
“Of course, there’s some people who don’t believe Covid-19 is a problem. I wish they could come to the Covid-19 ward, and work there for a week. I think they will be transformed.”