This article offers some personal insights into the Covid-19 situation in the country. One concern is that the public in some states behave as though the worsening outbreak is confined to the Klang Valley, or only to selected states.
This is a dangerous assumption as the situation is worsening in the whole nation. The lack of adequate data hampers the public’s appropriate response to the deepening crisis.
Cases Are Rising Rapidly All Over The Country
Figure 1 shows how fast the current outbreak is growing. While we took a year (2020) to reach 100,000 reported cases, it only took 22 days to achieve the same in May 2021.
We also know from the Ministry of Health (MOH) that clusters are no longer the primary focus, as unlinked community spread is rising. On May 11, 2021, Health diretor-general Dr Noor Hisham Abdullah stated that 80 per cent of cases are from the community.

It is important to recognise that numbers reported daily do not give the full picture as our testing is very limited, except perhaps for Selangor.
In the past, we averaged 40,000 to 70,00 total tests most days, but it was only in the last few days that 100,000 to 110,000 tests were done per day (114,027 tests on May 22, with 5.54 per cent positive). Tests probably picked up about 25 per cent of positive cases in the community.
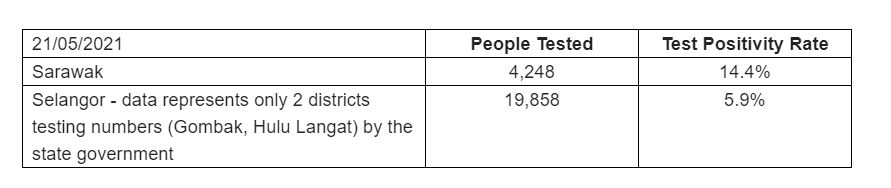
We have little access to testing numbers for each state, which would provide a better idea of what is happening. As an example, if you compare the testing numbers for Selangor and Sarawak for May 21, 2021, you can see the large disparity.
Much of the public is concerned with Selangor and think the outbreak is concentrated there. But note that the testing numbers for Selangor are huge compared to Sarawak, and the positivity rate for Sarawak is very high, indicating that testing is grossly inadequate (many positive cases missed).
Hence Selangor gets a ‘bad’ outlook with many cases, merely because they are testing extensively. Of all the states in the country, Selangor perhaps has the most accurate daily reported cases. We should be worrying about the other states.
ICU Bed Occupancy Is At Critical Levels Nationwide
While reported case numbers are not a good indicator of the real situation, ICU admissions (and deaths) can offer us a better understanding of what is happening in each state.
On May 21, MOH released data that Covid-19 intensive care (ICU) bed occupancy has increased from less than 200 beds in March to close to 900 beds on May 20.
This has only worsened in the past 48 hours. Again, there is a perception that this is a Klang Valley problem (MOH showed a table displaying ICU Covid-19 usage for the Klang Valley at 113 per cent on May 22).
However we have been made aware that nine out of 10 ICU beds nationally are occupied. Some state health departments have made available data on ICU bed usage for Covid-19 patients.
If you make a comparison, you can see that Malacca is the worst affected state. Sarawak is worse than Perak, even though parts of Perak have been placed under an Enhanced Movement Control Order (EMCO). All states should release Covid-19 ICU admission rates daily (remember that this will be affected by the number of deaths).
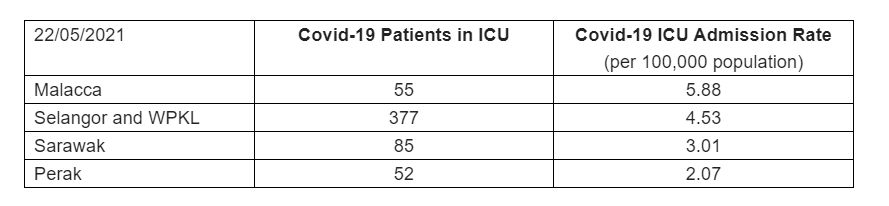
ICU beds are full (or exceeding 100 per cent) in the Klang Valley, Malacca, Sarawak, Penang, Kelantan, etc. Many private hospital ICU beds are also reaching maximum capacity.
In all states MOH has ‘repurposed’ other beds to turn them into ICU beds. Even coronary care unit (CCU) beds are being converted into ICU beds. Some patients are beginning to be ventilated in general wards.
It is critical to remember that ventilation and medical care in a repurposed bed and general bed is very different from what an ICU offers.
It is not just the ventilator that is important. There is the medical gas delivery system, plus all the supporting equipment (monitors, the number of perfusers, specialised bed, etc.).
The staffing is the most essential component. If you want to manage critically ill persons, you need one-to-one, ICU-experienced nursing care around the clock, a commodity which is very hard to find.
Hence, opening ‘new’ beds is difficult, and repurposed beds do not offer the same level of care.
Mortality Rate Is Rising
The number of Covid-19 patients dying is rising and the mortality rate is increasing; see Figure 2. In just the first 18 days of May 2021 we had 500 reported deaths, the same number we experienced in the whole of 2020.
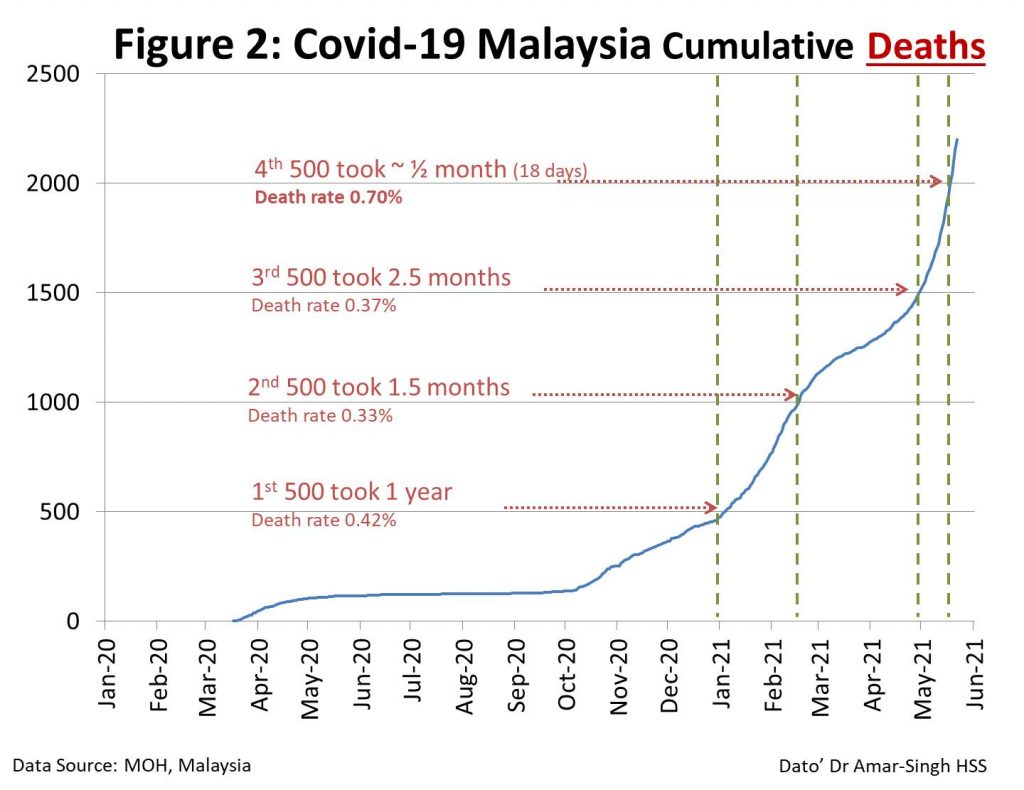
To give you a better understanding of this worsening crisis, allow me to use data from Sarawak. From January to April, there were 161 Covid-19 deaths reported.
However, from May 1 to 21, they had 86 deaths — comprising 53 per cent of all their Covid-19 deaths in 2021 (so far), occurring in the past 21 days. The same is happening throughout the nation.
Note that we had averaged a mortality rate of 0.3 to 0.4 per cent. But from May 1 to 22, the mortality rate rose to 0.7 per cent. (Sarawak’s mortality rate for May was 0.88 per cent).
This reflects our over-run ICUs, possibly more severe variants spreading and the huge size of our undetected pandemic. All states should make available Covid-19 mortality rates by month, so that the public can understand the crisis better and respond appropriately.
Remember also that ICU admissions and deaths lag behind the reported cases by two to three weeks. So what we are seeing now happened in late April to early May. This will worsen in the next few weeks due to movements during the recent Hari Raya holidays.
Younger Persons Are Dying And Mutations Spreading
Another changing trend is the increasing numbers of deaths among younger persons. In recent months, 20 to 30 per cent of all deaths occurred in patients under 60 years old (36 per cent in Sarawak from January to April).
In addition, increasing numbers of individuals are presenting at clinical Stages Four or Five (severe disease) which is worrying. This could be due to the increased spread of mutations (especially the South African variant), which have been detected in the Klang Valley, Kelantan, Perak, Sarawak, etc.
Our genome testing is limited, but it is likely that a sizeable proportion of the current outbreak is due to variants. These Variants of Concern (VOC) spread easier, are harder to detect, and cause more severe illness. This may explain the higher numbers, increased ICU bed usage, and younger persons dying.
When Will The Current Outbreak Peak?
We all want an end to the current wave, but we must realise that it has yet to peak. If we all work together, the current upsurge in cases could possibly peak in two to three weeks from now in West Malaysia.
However, in Sabah and Sarawak, the peak could occur in late June or early July, due to the impending Gawai and Kaamatan festivals. If these celebrations precipitate mass movement of individuals, it will make the current outbreak even worse.
We must remember the peaks do not signal the end of the current outbreak; sadly, there may be more to come. Our vaccination has been limited due to supply issues.
We have been informed that the bulk of vaccines will arrive from July onwards (in the second half of the year). Until we can vaccinate 60 to 70 per cent of the population, we will be open to even more waves.
What Are The Implications Of These Trends?
Quarantine centres are overflowing, and we will have to resort to home quarantine to cope. Existing quarantine centres are also far too congested and confined; many shy away from testing as they do not want to be admitted under these conditions.
Our ICU beds are already maxed out. The use of ‘repurposed’ and general beds for ventilation will increase mortality. We can expect more deaths during the next two to three weeks.
In addition, there is the sobering realisation that doctors might have to triage ICU bed access by age and prior chronic illnesses. We might be frustrated, but we must remember that our health care services have been underfunded and underdeveloped for decades. This has also happened in countries with better health systems like Italy.
We will also see an increased mortality in non-Covid-19 patients.
On many ‘normal’ days, we struggle to find ICU beds. Now, with so many ICU beds occupied by patients with Covid-19, those with other health needs that require ICU care will be affected. All states should make available non-Covid-19 mortality rates by month (compared to the pre-Covid-19 era).
What Can We Do?
The key is to avoid getting infected with Covid-19. Once infected, we run the risk of developing severe disease and long Covid. More than 10 per cent suffer from debilitating and incapacitating symptoms that can persist for months; some with permanent organ damage.
- Limit all unnecessary contact with others (except the family you live with). There is no safe number to meet at work, at religious gatherings, socially, at your home, etc. Avoid celebrating any festivals with others outside of your home and avoid any travelling.
- Work from home (if you can) as much as possible. No one is truly safe because of the extensive community transmission. Ideally work at home if possible.
- Online education for children. As a paediatrician, I am devastated by the damage this pandemic has done to our children, especially with the loss of schooling. But in the current crisis, keeping children at home and continuing their education there is the right move. Many children (40 per cent) have no digital devices. We need to work together to share our pre-loved devices with the more unfortunate members of our community, as well as invest in Chromebooks for them, which are cheaper than laptops.
- Focus on ventilation in all enclosed spaces. While we have been concerned with hand disinfection, which should be continued, we need to emphasise the need to improve ventilation in all building, including supermarkets, offices, shops, schools, etc.
- Improve the quality and fit of your mask. Most individuals wear a three-ply surgical mask, but this leaks at the side and limits our protection. Look online for good suggestions and videos on improving this. Two quick methods to improve your protection are to tighten your ear loops or wear a cloth mask over the surgical mask.
- Get vaccinated the moment you have a chance. While many of us are desperately waiting for our chance to get a vaccine, some who are eligible are hesitant. Please get any vaccine that becomes available, the moment you have an opportunity (including the AstraZeneca rollout). We also need to support old persons with registration, IT access and transport to help get them vaccinated.
- Help others. A significant portion of our community are struggling with daily needs, and we need to support them. Please share your resources with them.
- Maintain your personal physical, emotional, mental, and spiritual fitness. Together, we will overcome this adversity, but we have a long way to go, and we need to keep from falling into despair. Maintain good routines to keep you well, not just physically, but also emotionally and spiritually.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.




