KUALA LUMPUR, May 5 – Eating low-glycaemic index (GI) food may help reduce the risk of complications for diabetes patients, medical experts said.
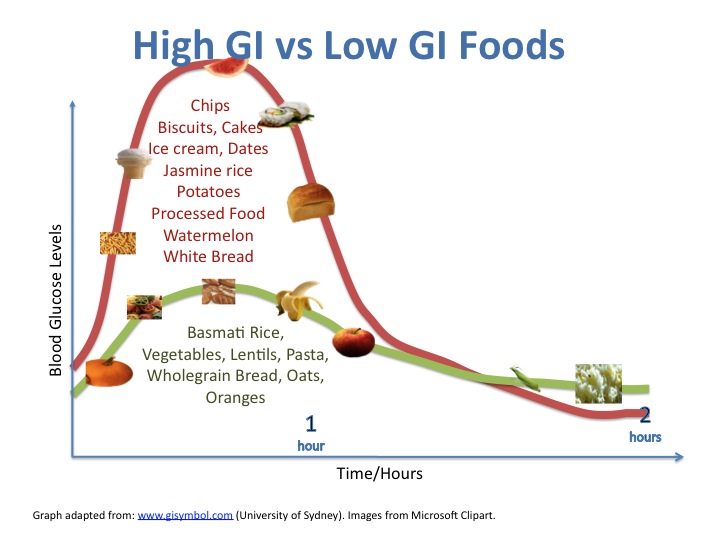
GI is a measurement on how fast or slow a food with carbohydrate can increase one’s blood sugar level. To put in simple terms, low-GI foods are absorbed slowly, whereas high-GI foods are absorbed fast.
“Recent investigations show that good glycaemic control decreases the risk for diabetic complications in type 2 diabetes patients,” Health deputy director-general (public health) Dr Chong Chee Kheong told CodeBlue recently.
“Poorly controlled diabetes increases the risk for skin, bone, eye, ear, gastrointestinal, urinary tract, and respiratory infections, among others, with significantly increased hospitalisation and mortality rates.”
The Glycemic Index Foundation (GIF) classifies food on a range until 100 to distinguish the speed at which a particular food increases one’s blood sugar level. Foods that record under 55 are low GI, as they release sugar into the bloodstream slowly. GI ratings at 56 to 69 are classified as medium, while foods with GI ratings at 70 or above are classified as high-GI food.
A slower release of sugar into the bloodstream helps to avoid high sugar content in the body and, therefore the likeness of being diabetic is significantly reduced.
“Indeed, low-GI food provides benefits in terms of controlling blood glucose and likely delaying or reducing the rate of diabetes,” Dr Chooi Kheng Chiew, consultant endocrinologist and physician at KPJ Ampang Puteri Specialist Hospital, told CodeBlue.
“The slower release of glucose into the circulation mitigates the glucotoxicity that high blood glucose levels exert on the pancreatic beta cells.”
Studies Show Low-GI Diets May Lead To Weight Loss
A systematic review and meta-analysis of 54 trials, published in The American Journal of Clinical Nutrition in 2019, found that low-GI diets had the potential to control blood glucose, in combination with pharmacological and lifestyle interventions.
The review also noted that the reduction of fasting blood glucose and glycated hemoglobin (HbA1c), which is a form of hemoglobin to which glucose is bound, in people with diabetes who ate low-GI diets suggested a possible improvement in insulin sensitivity, “a significant achievement for a dietary intervention”.
“Low-GI diets may be useful for glycaemic control and may reduce body weight in people with prediabetes or diabetes,” the analysis concluded.
Sarah Blake, a PhD student at the University of Bristol, wrote in the British Journal of General Practice last February that after being diagnosed with type 1 diabetes, she was careful about how she ate high-GI foods and combined higher-glycaemic sugary and starchy foods together with unsaturated fats, proteins, or fibre, while maintaining her insulin regime. Her blood sugars quickly dropped to below 7 mmol/L, the level at which diabetes is diagnosed.
“Our language tends to focus on ‘weight’ or ‘calories’, both measurable variables. But ‘low-calorie’ foods do not always equate to a ‘low-glycaemic’ index. As a result, we may miss out on opportunities to adjust our diets and balance our blood sugar,” Blake wrote.
She pointed out that many average or underweight people are unaware that they are at risk of diabetes, citing research from the UK’s National Diabetes Programme 2017/2018 that found 15 per cent of patients with elevated blood sugars, with a HbA1c greater than 42, had a body mass index (BMI) below 25.
“Risk factors often include weight, age, ethnicity, and blood pressure. High-glycaemic diets or blood sugar spikes are curiously absent from these lists, despite being linked as a cause of type 2 diabetes,” Blake said.
Blake, who worked with pre-diabetic patients, found that replacing high-GI foods with lower glycaemic alternatives – along with changing food ratios and avoiding starch and sugary foods in isolation or before going to bed – often seemed to reduce their blood sugar levels.
Study Shows Poor Knowledge On GI And Diabetes
MOH’s National Health and Morbidity Survey (NHMS) 2019 found that diabetes (sugar level at 7.0 mmol/L or more) prevalence among Malaysian adults increased from 13.4 percent in 2015 to 18.3 per cent in 2019.
“Diabetes is a major public health concern in Malaysia, and the prevalence of type 2 diabetes has escalated to 18.3 per cent in adults above the age of 18, based on NHMS 2019,” Dr Chong said.
Interestingly, the prevalence of diabetes also varies among the three biggest ethnicities in Malaysia.
“The prevalence of diabetes varies among the major ethnic groups in Malaysia, with Asian Indians having the highest prevalence of T2D, followed by Malays and Chinese,” said Dr Chong.
One major reason for this is the lack of awareness on the prevalence of diabetes and the importance of healthy diets.
In 2020, a study was done by a group of researchers from Universiti Putra Malaysia (UPM), with the support of the Ministry of Science, Technology and Innovation (MOSTI), to gauge the level of understanding and knowledge on the GI concept among Malaysian women with gestational diabetes. Gestational diabetes is diabetes diagnosed for the first time during pregnancy.
The study recorded only 11.8 per cent of respondents having a good level of knowledge of the disease and the concept of GI; while more than a quarter of the respondents (25.9 per cent) had poor nutrition knowledge levels.
On the other side of the spectrum, Malaysia’s overweight and obesity problem is also seeing a rising trend in recent years. The World Health Organization (WHO), in 2019, said that Malaysia is the fattest nation in Asia, and ranks second in ASEAN countries for obesity among children aged 5 to 19 years.
The NHMS released in 2019 also echoes this, with new revelations that obesity prevalence among Malaysian adults increased from 17.7 per cent in 2015 to 19.7 per cent in 2019.
“The increase in the prevalence of overweight and obesity has contributed significantly to the parallel increase in the prevalence of Type 2 Diabetes,” Dr Chong said.
“The overall prevalence of abdominal obesity in Malaysia, measured by waist circumference, has been reported between 55.6 per cent and 57.4 per cent.”
Eat Healthy, Monitor Blood Sugar Levels Regularly
In 2019, the government introduced an excise duty on sugar-sweetened beverages. This was fixed at 40 sen per litre for carbonated drinks containing sugar exceeding 5g per 100ml, as well as on fruit and vegetable juices containing sugar exceeding 12g per 100ml.
The effort to eat a healthy diet, keep tabs on blood sugar levels, and in turn stay away from diabetes, is the responsibility of every individuals, say experts.
Dr Chooi opined that regular monitoring of blood sugar level is essential in encouraging Malaysians to adopt a low-GI diet.
“If a person performs regular blood glucose monitoring, or continuous glucose monitoring, he or she is able to see the impact foods of varying glycaemic index can have on their blood glucose levels, and this can promote healthy food choices.”