KUALA LUMPUR, Dec 2 — Chronic conditions and mental illness were more common in the poorest, unemployed people, and homemakers in Malaysia, said Khazanah Research Institute (KRI).
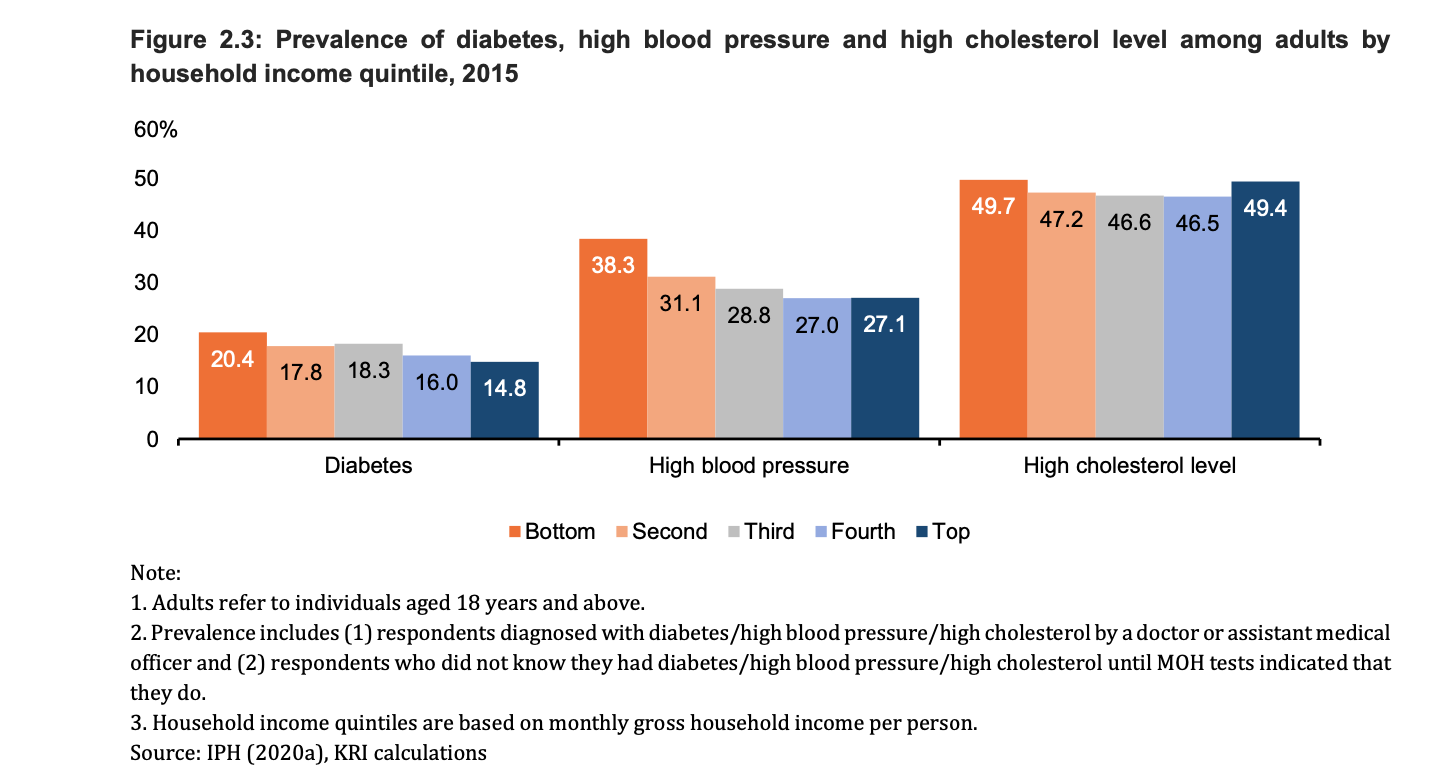
According to a report by KRI titled “Social Inequalities and Health in Malaysia” published yesterday, the prevalence of non-communicable diseases (NCDs) for 2015 was highest in the bottom 20 per cent (B20) of income earners. For example, the prevalence of diabetes in the B20 group was 20.4 per cent, 1.4 times higher than the top 20 per cent (T20) of income earners.
High blood pressure was seen highest in the B20 group (38.3 per cent), followed by those in the second lowest quintile of household income earners (31.1 per cent), third quintile (28.8 per cent), fourth quintile (27.0 per cent), and the T20 group (27.1 per cent).
The prevalence of high cholesterol was also top in the B20 group (49.7 per cent). However, the T20 group also had a high prevalence of high cholesterol levels of 49.4 per cent, only 0.3 per cent lower than the B20 group.
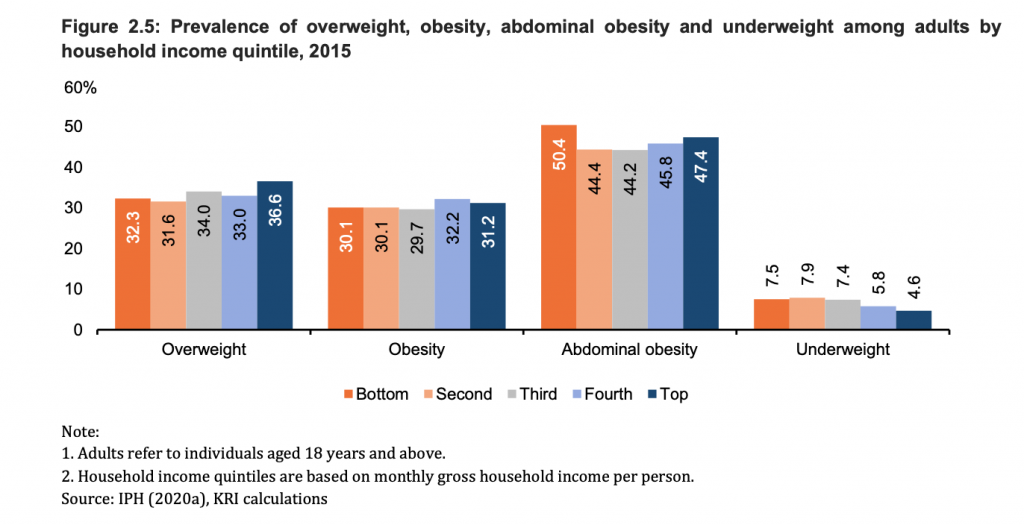
On the other hand, the prevalence of being overweight was seen highest among the T20 group with a prevalence of 36.6 per cent, while the prevalence of abdominal obesity was seen highest in the B20 group (50.4 per cent), followed by the T20 group (47.4 per cent).
The prevalence of underweight was concentrated in lower income quintiles. A total of 7.5 per cent of adults in the B20 group were underweight, while only 4.6 per cent in the T20 group were underweight.
KRI’s report said obesity was increasing at a faster rate among the poor, and not that the prevalence of overweight and obesity is declining among the rich. One reason for this is that the well-off are better and able, thus, more prone to adopting health-promoting habits than the poor.
For example, the consumption of healthy foods is partially dependent on the financial ability to purchase them. A survey of 1,719 adults throughout Malaysia revealed that one barrier to practicing healthy eating habits is the price of healthy foods.
As a result, studies have shown that poorer communities consume more of cheaper energy-dense and nutrient-poor diets, which is a global phenomenon.
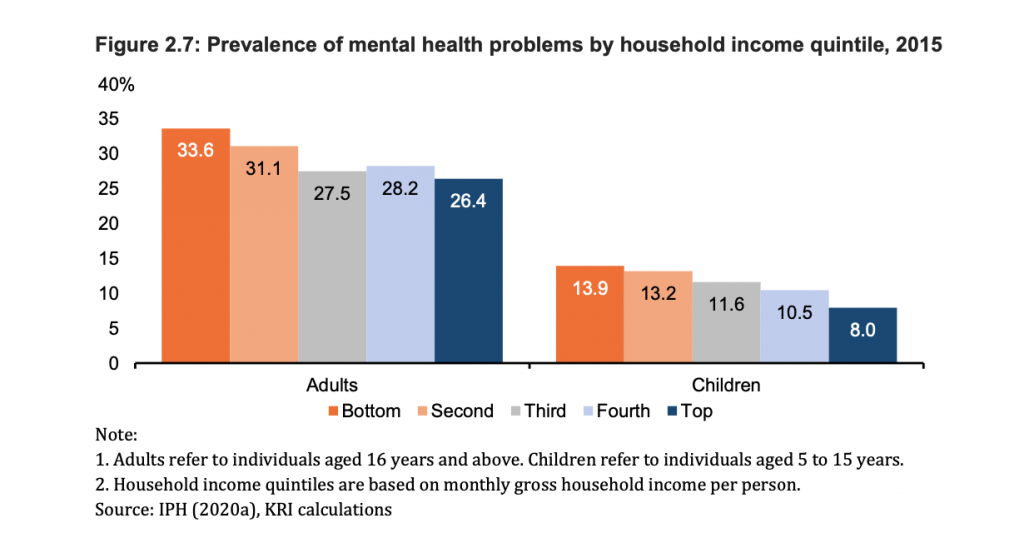
Moreover, the prevalence of mental health problems in 2015 among both children and adults were seen highest in the B20 group (33.6 per cent) and lowest in the T20 group.
The pattern was the same in children between the age of five and 15 years, as the highest prevalence of mental illness was seen in the B20 group and lowest in the T20 group.
It was noted by KRI that disadvantaged people experience far more insecurity and stress in their lives.
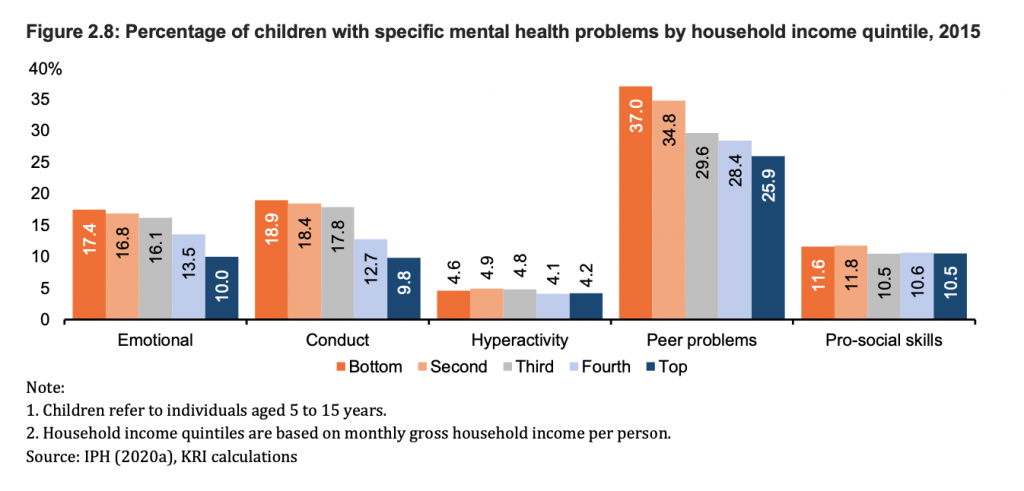
Children with peer problems, including those who tend to be more solitary or are bullied by their peers, were seen more concentrated in the B20 group. Similarly, those with emotional problems (children who feel unhappy and often worry), problematic behaviour (those who cheat and lie), hyperactivity, and lack of pro-social skills were seen highest in B20 children.
Prevalence Of NCDs And Mental Illness Highest In Unpaid Workers, Homemakers
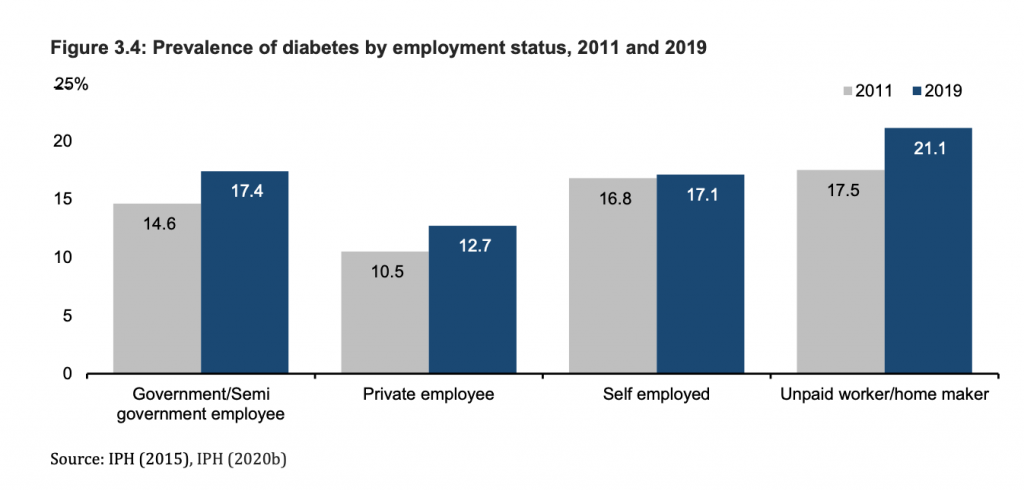
In 2019, the prevalence of diabetes among unpaid workers or homemakers were the highest (21.1 per cent), as compared to government or semi-government employees (17.4 per cent), self-employed (17.1 per cent), and private sector employees 12.7 per cent).
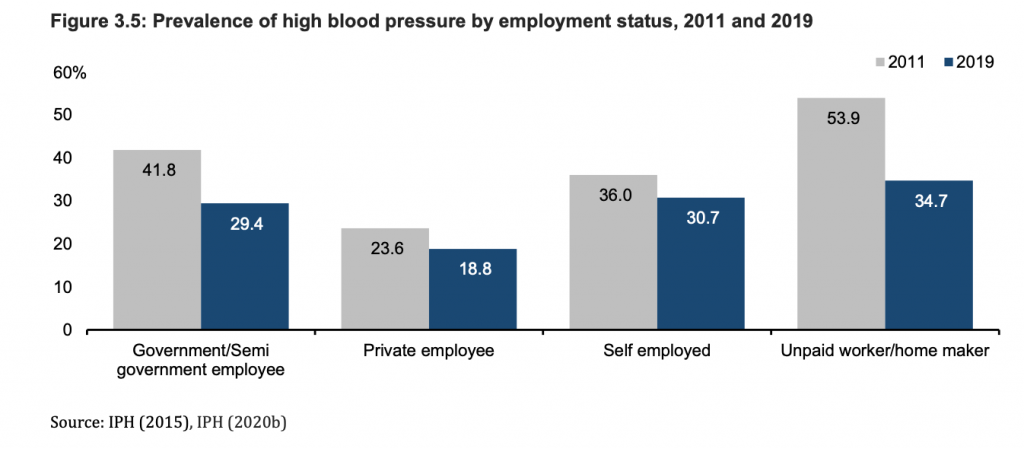
Although the prevalence of high blood pressure by employment status between 2011 and 2019 decreased across all categories, the prevalence of high blood pressure last year was the highest at more than a third of the unpaid workers or homemakers group (34.7 per cent).
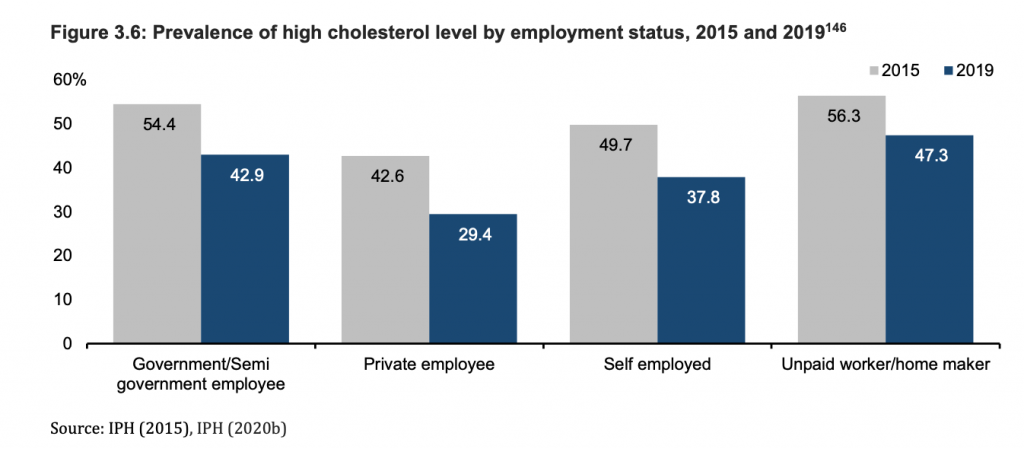
A similar pattern was seen for high cholesterol levels, which was also highest in unpaid workers or homemakers at nearly half (47.3 per cent) in 2019.
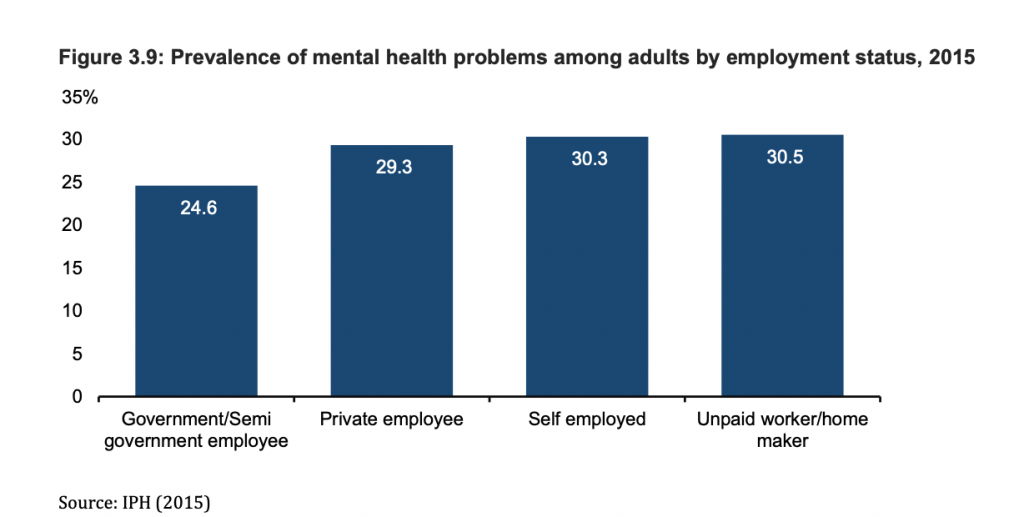
In 2015, the prevalence of mental health problems were the highest for unpaid workers or homemakers (30.5 per cent), followed by the self-employed (30.3 per cent) and private employees (29.3 per cent), and lowest in government or semi-government employees (24.6 per cent).
KRI found that loss of employment has significant long-term detrimental effects on both mental and physical health. The negative health effects of unemployment was also strongly associated with the duration of being unemployed.
The unemployment rate in Malaysia has remained low and stable over the past decades. However, following the Covid-19 pandemic, unemployment rates rose in the beginning of March during the implementation of the movement control order (MCO).
Malaysia’s unemployment rate peaked at 5.3 per cent in May 2020 and has since shown signs of recovery, with a reported unemployment rate of 4.7 per cent in August 2020. However, the third wave of the Malaysian coronavirus epidemic may have worsened unemployment rates in Malaysia, KRI noted.
B20 Likely To Use Government Facilities For Both Major And Minor Health Problems
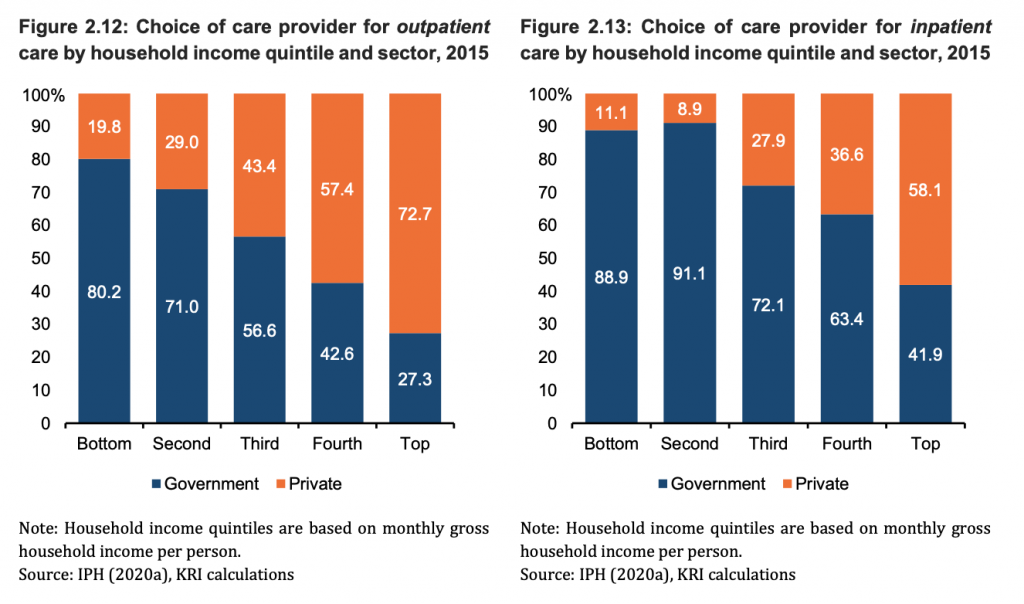
According to the National Health and Morbidity Survey (NHMS) 2015, lower income quintile groups, especially the B20, said they were likely to visit government health facilities for minor conditions like flu, fever, cough, and stomach ache, while private facilities were the main choice among those in the fourth income quintile and the T20.
However, for major health problems like cancer, diabetes, and cardiac problems, all income groups preferred to use public over private health facilities.
In the 2015 NHMS, respondents perceived that the average cost to treat major health problems in private health facilities were much higher as that of government health facilities. For example, in 2015, the average perceived cost of coronary bypass surgery in a government facility was about RM2,144, but it was six times higher in a private health facility (RM13,124).
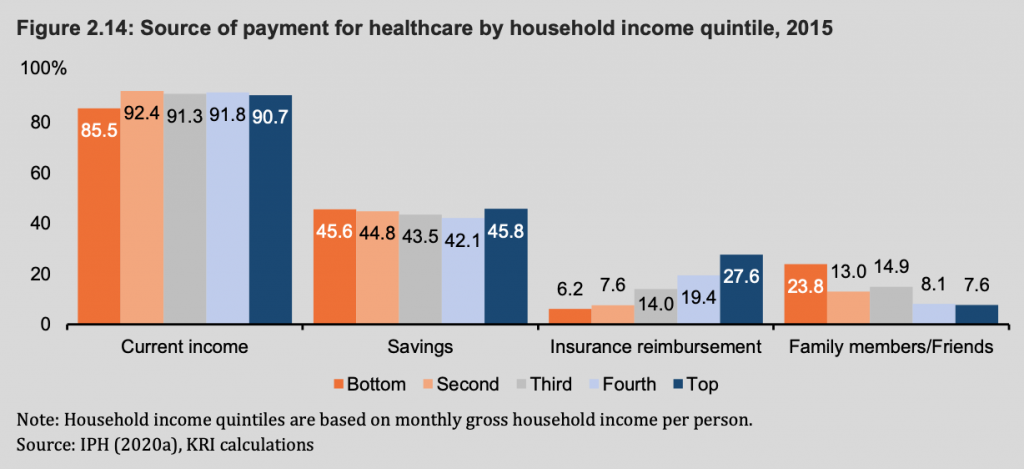
KRI also found that most Malaysians used their own incomes and savings to pay for expenses related to health care. The T20 group used insurance reimbursement as a source of payment at a rate of three times higher than the B20 group.
The B20 group relied more on informal social networks, such as help from family and friends, to pay for health care expenses.