Before the year 2020, you might have visited an anaesthesiologist if you needed to undergo surgery. Typically, after the visit, you would feel less anxious and reassured that you will be well taken care of while you are asleep during the surgery.
After the surgery, you would most likely return to your everyday life, not remembering much about this unassuming person because the anaesthesia was uneventful, precisely as it should be. This is what any patient undergoing anaesthesia for surgery has come to expect.
Fast forward to today, mention an anaesthesiologist and the response might be different. Anaesthesiologists all over the world are emerging conspicuously in the public in a most startling manner; featured on the front page of TIME magazine, hailed as “special heroes” by international news outlets and acknowledged by the Director-General of Health Malaysia on multiple occasions as vital frontliners in our war against Covid-19.
This is because anaesthesiologists have been called to the front lines to perform two lifesaving and dangerous procedures: endotracheal intubation and operation of ventilators, a life support machine.
These procedures are essential to ensure patients who are fighting for their breath can receive mechanical breathing and oxygen therapy. Very urgently and rapidly, anaesthesiologists find themselves reassigned from operation theatres to intensive care units, isolation wards and operation theatres dedicated to treating Covid-19 patients, shouldering the burden of caring for the sickest of the sick.
During the initial phase of the pandemic, before we fully understood how infectious and deadly Covid-19 is, we anaesthesiologists accepted this frontline assignment despite a shortage of equipment, risking our own health in the call of duty.
In conjunction with the National Anaesthesia Day 2020, we wish to shed light on the role and experiences of frontline anaesthesiologists during the pandemic. What is ‘endotracheal intubation’ that we so often read about in the news? And what has the pandemic meant for the anaesthesiology and critical care fraternity?
Endotracheal Intubation
Endotracheal intubation is the process of inserting a breathing tube through the mouth into the trachea or windpipe. Once intubated, the breathing tube is then connected to a ventilator which delivers lifesaving oxygen to the lungs.
Without this intervention, a patient is unlikely to survive severe Covid-19 lung infection. Endotracheal intubation is also a necessary medical procedure for patients undergoing general anaesthesia for surgery.
What is so dangerous about endotracheal intubation? The procedure triggers a generation of small aerosols infected with the virus, which can be transmitted to the anaesthesiologist and persons nearby. Moreover, most operation theatres are positive air pressure environments, which means viral aerosols can spread further.
The safety of health care workers is one of the top priorities in ensuring the continuation of health care service during this pandemic, not only for patients suffering from Covid-19, but also for patients with non-Covid-19 related diseases. Hence, it is of paramount importance that we ensure endotracheal intubation is safe for the anaesthesia team.
Embracing New Normals In Anaesthesia Practice
Anaesthesiology teams, across the world, are now changing the way they perform intubation to make it safer for everyone involved.
First and foremost, anaesthesiologists must wear appropriate personal protective equipment (PPE) when carrying out medical procedures involving airways, including with non-Covid-19 patients, as they may be asymptomatic carriers.
This practice was almost unheard of in daily clinical work ten months ago. Today, to don (put on) and to doff (take off) PPEs correctly to avoid self-contamination is a daily routine.
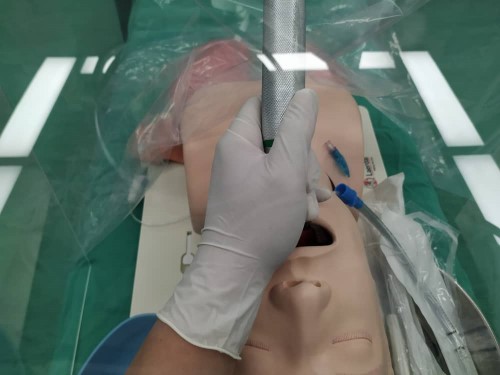
An innovative piece of protective equipment for anaesthesiologists now frequently seen on social media is the aerosol intubation box. It is an acrylic box placed over a patient’s head with holes for the anaesthesiologist to access a patient’s mouth during endotracheal intubation.
Since the beginning of the pandemic, we learned that while it is effective in containing aerosolised droplets, the boxes can make intubation more difficult to perform. However, as patients who had undergone surgery early on in the pandemic were not required to do Covid-19 tests, the intubation box did serve its purpose as an important piece of protective equipment.
Another piece of medical equipment revolutionising anaesthesia practice is the videolaryngoscope (VLS), a medical device equipped with a camera that allows indirect visualisation of the airway, allowing the anaesthesiologist to maintain a safe distance away from the patient’s mouth.
In contrast, the conventional laryngoscope requires the anaesthesiologist to have direct visualisation of the airway. The face of the anaesthesiologist needs to be mere inches away from the patient’s mouth.
Prior to this, VLS was reserved for use only in especially difficult cases. Due to its high costs, it was considered a “luxury” item that was not readily available; in fact, many hospitals had only one or none at all. This pandemic has been a catalyst for the use of VLS as the first-line option for endotracheal intubation for all patients.
The highly specialised world of anaesthesia, pain medications and care for the critically ill patients often go unnoticed by the public. Anaesthesiologists frequently play the role of guardians in ensuring patient safety in the complex medical environment that goes beyond the operation theatres.
Anaesthesiologists are also trained to stay calm, think fast, and stay focused and purposeful in crisis situations. They work as a team, ensuring each member fulfils their role during a crisis.
These attributes have taken most patients through anaesthesia and surgery, one of the greatest physiological stresses to a body, safely, proving that during a pandemic, anaesthesiologists can be relied upon to do their job and save lives.
The Malaysian Society of Anaesthesiology (MSA) will be hosting a webinar on “Occupational Wellbeing and Patient Safety” in conjunction with National Anaesthesia Day at 10AM on 17 October 2020. Stream it live on MSA’s Facebook Page.








