The smarter of the two writers kick-started this conversation by asking: “Why has nobody produced CIG [coronavirus immunoglobulin] like MIG (not Russian jet-fighters but Measles Immunoglobulin) or VZIG (Varicella Zoster Immunoglobulin or antibodies against chicken pox or shingles). Isn’t it a low hanging fruit?”
And so the journey of sourcing for evidence of this modality of intervention began.
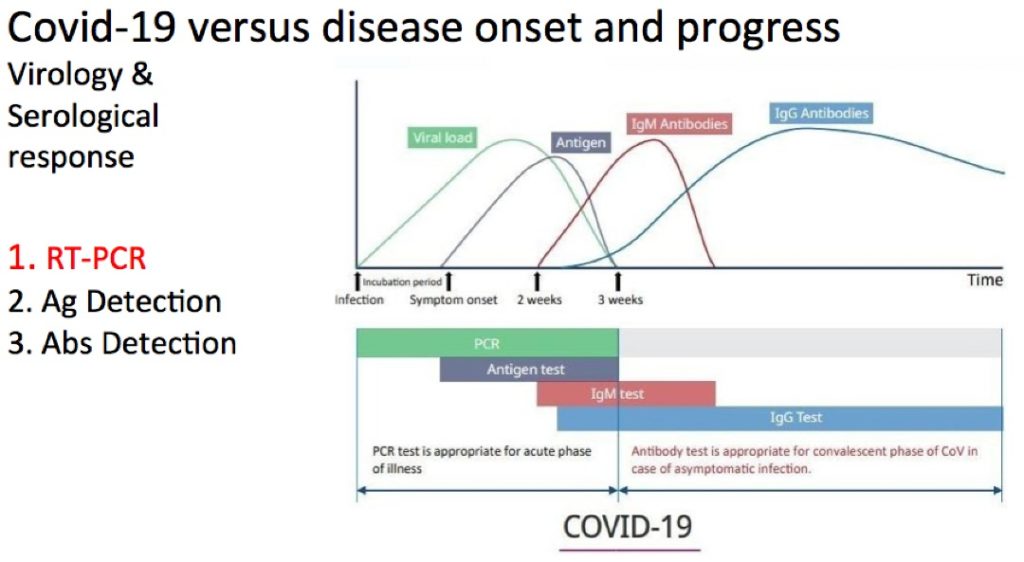
The body’s immune system makes antibodies in response to an attack by bacteria and viruses. It might be 14 days onwards for the body to produce IgM and later IgG antibodies against the SARS-CoV-2 (see graph).
This is called active immunity and can last many years. And for antibodies against viruses like measles, mumps, rubella and chicken-pox, it can last a lifetime.
Vaccines, through the administration of weakened viruses, dead bacteria or toxoid ramps up antibody production and also induces active immunity. The immunity is long term, even lifelong because the antigens in the vaccine triggers the memory cells in the immune system, which are able to immediately produce protective antibodies when faced with the pathogen again.
Doctors can harvest the antibody-rich plasma from the convalescent patient. It can be administered immediately to prevent or treat infection in another infected patient. This is called passive immunity. The antibody proteins will only last from a few weeks to a few months.
This has already been used to treat measles and varicella (chicken-pox) patients with measles immunoglobulin (MIG) and varicella zoster immunoglobulin (VZIG).
Eleven critically ill Covid-19 patients in New York and Houston has been treated with Coronavirus Immunoglobulin (CIG) since 28 March 2020. The U.S. Food and Drug Administration (FDA) authorised its emergency use, utilising plasma from other patients who have recovered from the coronavirus infection.
This is part of the National Covid-19 Convalescent Plasma Project to study whether convalescent plasma can prevent infection in people exposed to Covid-19 against a placebo.
A second trial will study whether plasma can prevent moderate Covid-19 disease from becoming severe and requiring intensive care and a third will study whether the therapy helps the most critically ill patients.
Convalescent plasma were used in 2003 SARS-CoV1 and 2013 MERS-CoV outbreaks. They showed benefit, but the intervention was not controlled with a placebo arm.
In Shenzhen, China, five patients were successfully treated with CIG. Three have been discharged and two are in stable condition. But, they had also gotten antiviral medications, so it’s unclear which therapy, if any, was the critical success factor.
The Spike Protein (SP) on the coronavirus, pierces and invades the human cells, taking over the cell processes to make many copies of itself. The thinking is that the antibodies sticks itself to the virus, destroys it, thus preventing the SP from binding to the human cell, preventing it entry, thus blocking infection and cloning itself in the human cells.
There is now an unprecedented global initiative to research the efficacy and safety of various antiviral agents against SARS-CoV-2 in the WHO-led SOLIDARITY trial.
Finally, there are at least 30 coronavirus vaccine candidates in the pipeline. Two are already in phase one clinical trials in the US and China. It would be the game changer, the panacea in our efforts to short-circuit the Covid-19 pandemic by boosting the herd immunity thus preventing more morbidities and mortalities and extinguishing the outbreak.
It is a long time coming, earliest 12-18 months, and meanwhile CIG is an interim measure to prevent infection in exposed persons, prevent progression and/or mitigate the criticality of the sickest patients.
Adjunct Prof Dr Musa Mohd Nordin is a paediatrican. Prof Dr Wan Ariffin Abdullah is a paediatric haemato-oncologist.
- This is the personal opinion of the writer or publication and does not necessarily represent the views of CodeBlue.





