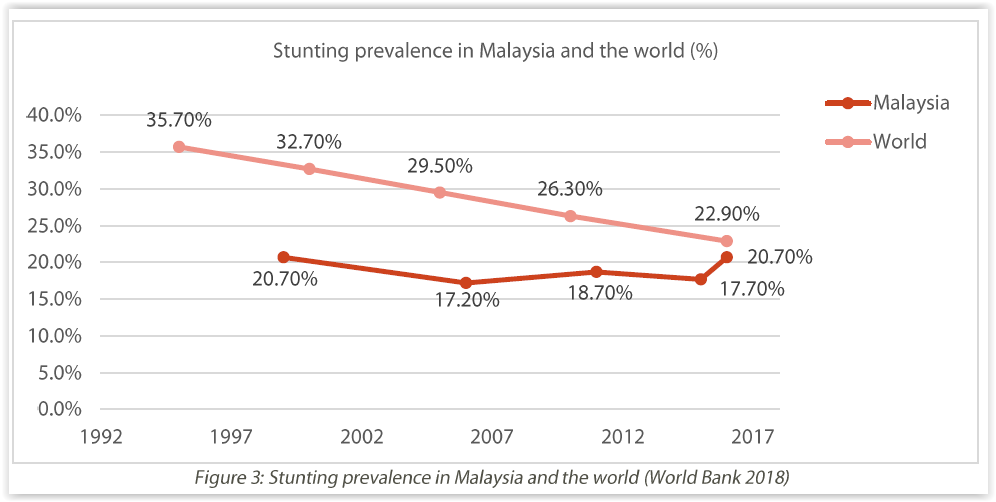
KUALA LUMPUR, May 17 — Two out of 10 Malaysian children below five are stunted, far worse than the 7 per cent prevalence in conflict-ridden West Bank and Gaza, a study showed.
The shocking study by Derek Kok — a research associate at the Jeffrey Cheah Institute on Southeast Asia and the Jeffrey Sachs Centre on Sustainable Development — also revealed that the stunting rate in Malaysia actually worsened over the past decade to its 1999 level of 20.7 per cent.
Malaysia’s stunting rate of about 21 per cent, according to the 2016 National Health and Morbidity Survey (NHMS), was three times higher than the overall 7 per cent prevalence that year in upper middle income countries, of which Malaysia is one.
“Stunting can adversely affect the health, education, and productivity outcomes of children. It has potentially serious social and economic costs for the overall development of the country,” Kok wrote in his study titled “Stunting in Malaysia: Costs, causes, and courses for action” released this month.
Malaysia’s stunting prevalence was even higher than lower middle-income countries like Ghana (19 per cent) and comparable to Iraq’s stunting rate of about 23 per cent at the end of the American invasion in 2011.
Children’s stunting in Malaysia cut across income levels and ethnic groups, and were equally prevalent in both cities and villages. Malaysia’s 21 per cent stunting rate exceeded the 11 per cent target set for 2025 under the National Plan of Action for Nutrition of Malaysia 2016 to 2025.
Stunting — children’s inability to reach their potential height for their age — is the most common measurement used to identify chronic malnutrition.
Almost one-third, or 30 per cent, of children below five in the poorest households in Malaysia that earn below RM1,000 monthly are stunted. But stunting prevalence is also high at about 17 per cent in families with a household income of above RM5,000 a month, compared to the 7 per cent rate in other upper middle income countries.
Malaysia’s poorest state of Kelantan recorded the highest prevalence of stunting at 34 per cent, followed by Terengganu (26 per cent), and Pahang (26 per cent). Kuala Lumpur’s stunting prevalence was the lowest in the country at about one out of 10 children below five. Almost two out of 10 children below five in Selangor, Malaysia’s richest state, were stunted at about 19 per cent.
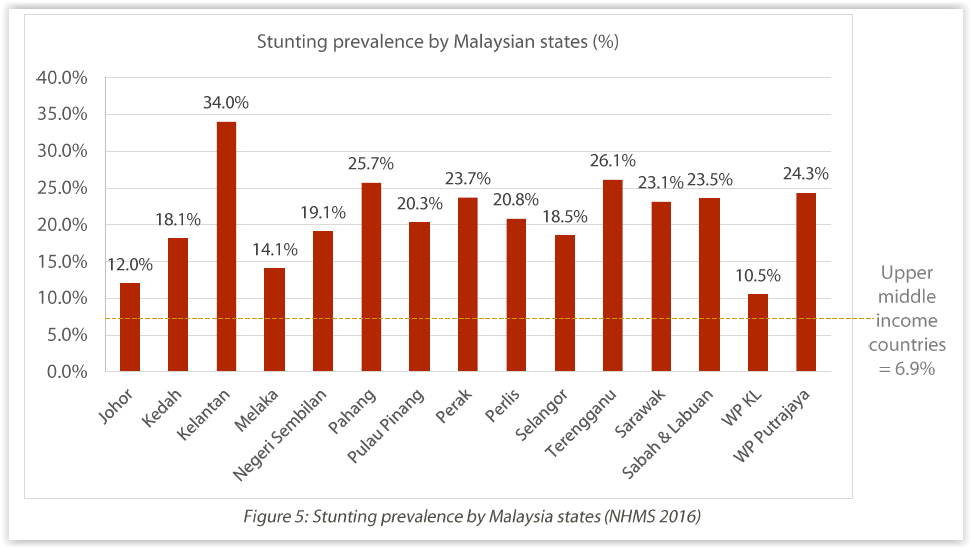
The stunting rate in urban and rural areas was roughly similar at about 19 per cent and 23 per cent respectively.
About one out of four non-Malay Bumiputera children under five was stunted, compared to Malays (21 per cent), Indians (17 per cent), and Chinese (14 per cent).
Kok cited a Unicef study that found 12 per cent of children living in low-cost flats ate less than three meals a day. Almost all of these households, or 97 per cent, cited high food prices for not preparing healthy meals for their children.
Almost two out of 10 Malaysian children aged six to 23 months did not eat at least two meals a day, according to the 2016 NHMS.
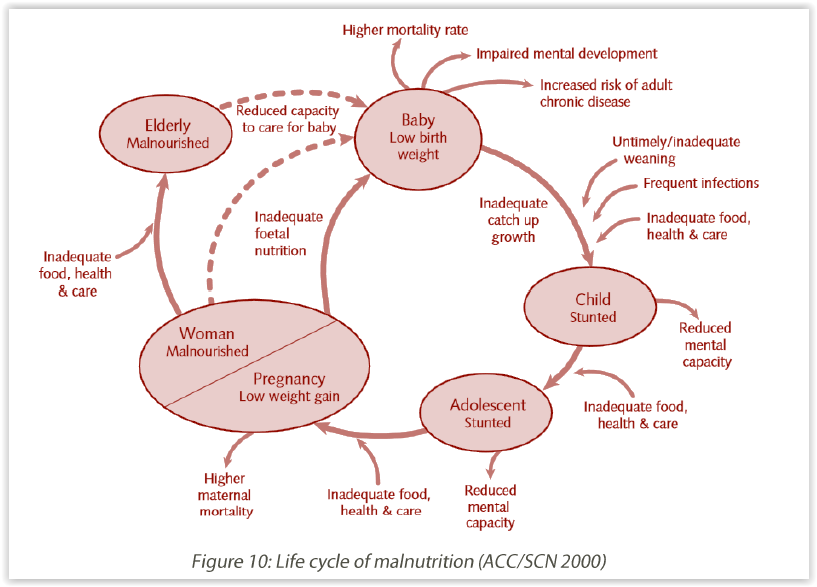
About a quarter of Malaysian women of reproductive age suffered from anaemia in 2016, while the prevalence of anaemia in pregnant women was about 37 per cent that constituted a “moderate public health problem”. Only about 69 per cent of women were booked for antenatal visits in the first trimester, according to the 2016 NHMS.
Almost 10 per cent of Malaysian children below five years were of low birth weight, compared to about 6 per cent prevalence in other upper middle income countries. Malaysia’s prevalence of low birth weight has not reduced much since 2007’s 11 per cent rate.
The study also highlighted a lack of awareness in Malaysia about child stunting, pointing out that only 6.6 per cent of Malaysian adults were health literate.
According to the research, stunting could lead to higher risk of death and disease from infections like diarrhoea in the short-term, besides heightening the risk of adult obesity in the long-term.
Kok cited studies in other countries that showed lower schooling rates and poorer educational performance among stunted children.
He said children’s stunting must not be viewed in isolation, but seen as part of the malnutrition life cycle as mothers’ and girls’ health and nutrition was equally important.
“Addressing stunting is also an important step in tackling Malaysia’s ‘triple burden of malnutrition’ — obesity, anaemia, and stunting — which threatens to grow into a public health emergency.”
Kok urged the Malaysian government to introduce a universal cash transfer programme targeting all children below two years, noting that stunting was high across all income levels, not just among the bottom 40 per cent (B40).
He cited Unicef’s calculations that an RM200 monthly universal transfer would not reach 1 per cent of Malaysia’s GDP, as he called for money to be diverted to this scheme from the upcoming sugar tax and other sin taxes and from reallocating fuel subsidies.
“As it stands, choosing not to invest in children is simply not a good economic decision,” he said.
The study also urged the prime minister to chair the steering committee of the government’s proposed National Children’s Wellbeing Roadmap. “Senior” ministries like the Finance and Economic Affairs Ministries should also be involved.
The research further called for the establishment of a bipartisan Parliament standing committee to monitor the implementation of the National Children’s Wellbeing Roadmap.